Embracing the Power of Talking: Why Therapy is Key
Oh, the absolute power of talking. Yes, it's neither an ancient secret nor a modern remedy, but a blend of the two in the most beautiful manner. You see, long before medical doctors even existed, there were people, good listeners, willing to lend an ear, offer a shoulder, or utter words of comfort to the ailing or troubled one. With time, this act of healing has evolved and gained the importance it rightfully deserves, creating a niche for itself under the spectrum of therapy and counseling. One might ask, 'But Natalie, how does this aid in managing proctitis?' I have answers, and I promise you, they’re as enlightening as a sunny day in Melbourne.
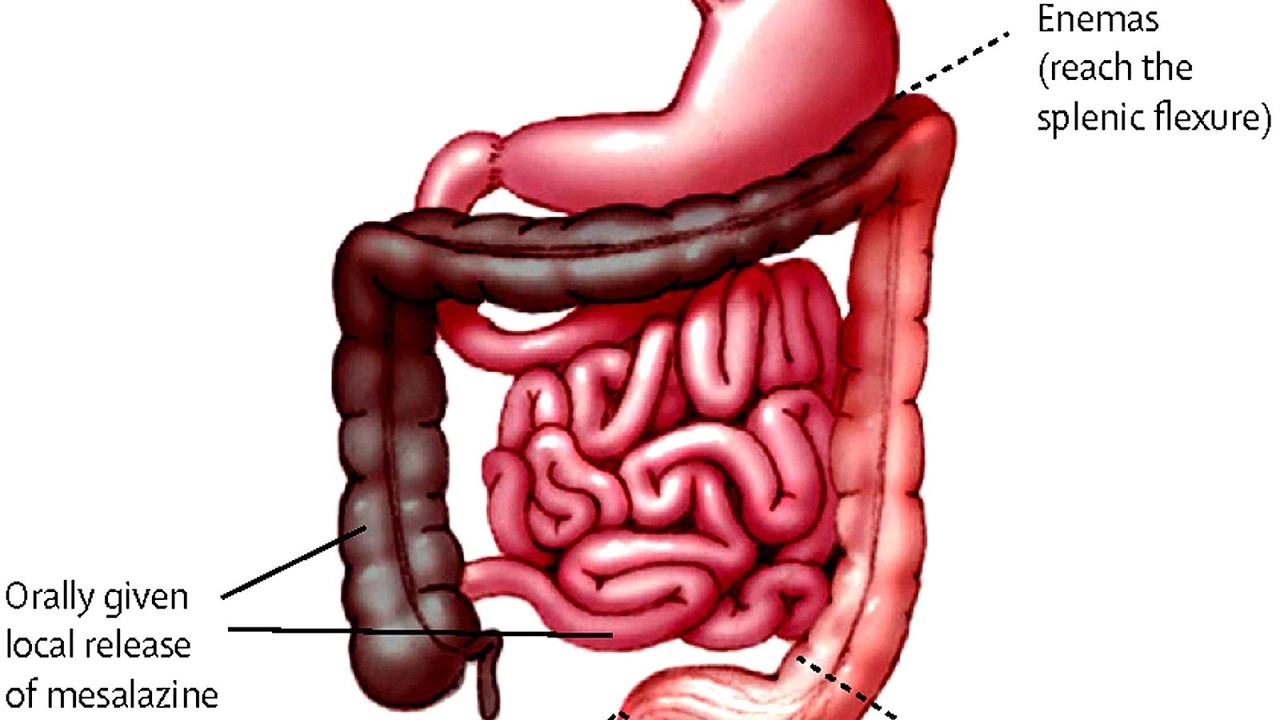
In simple terms, proctitis is inflammation of the rectum lining, which can cause discomfort, bleeding, and a spree of other embarrassing symptoms. It's that daunting subject we often detour around, but the fact is, nothing makes you appreciate the phrase 'pain in the butt' more than proctitis. It's not something you'd openly discuss while lounging on a couch sipping your favorite cup of tea. However, truth be told, it's these moments of open conversations that we need to bring into practice, breaking the stigma and silence surrounding such conditions. And that's exactly where therapy and counseling step in.
Nurturing Mind-Body Connection: Unleashing Inner Healing Capabilities
The human mind is an intriguing space, isn't it? Constantly buzzing with thoughts, it carries the potential to impact our overall well-being significantly. I find this utterly fascinating. It's as if we are carrying an incredibly intelligent life adviser within us. How often do we take the time to understand our body signals? How often do we listen to our inner counsel patiently? Well, therapy and counseling essentially prompt us to do that.
By employing therapeutic practices, we can learn to respond and not react, alleviate stress, focus on positive thinking, and most crucially, develop a deeper understanding of our body's signals. This mindful approach translates into effective management of health conditions, including proctitis. There's compelling evidence that chronic inflammation is often tied to stress and anxiety. By addressing our mental health, we can support our body to handle, manage, and ease the physical symptoms of proctitis, and isn’t that a good thing?
Reconstructing Negative Perceptions: Transforming Distress into Triumph
Like it or not, diseases often come with added luggage - emotional and psychological distress. It's like buying a pair of shoes, but instead of free socks, you get anxiety or stigma. This emotional upheaval is usually underplayed in the face of physical discomfort, but the fact is, it significantly affects your healing process. Think of it as having a bad internet connection while trying to stream a blockbuster movie - truly the stuff of nightmares.
And this is why I call therapy the unsung superhero. Though it doesn't come with a cape, it surely swoops in to save the day. Through cognitive-behavioral therapy, mindfulness, stress reduction techniques, and talking therapy, we can effectively challenge and reconstruct any negative perceptions surrounding proctitis. You see, the disease itself can't be labeled as 'bad'. It's our view of it that sequences the increase or decrease in its impact on our lives. It’s about transforming the distress into a journey of understanding, acceptance, and triumph. As someone who's juggled life in Melbourne with chronic health issues, trust me, therapy is like a box of chocolates, utterly soothing.
The Allied Support: A Personal Story
Personally, I have found therapy and counseling to constitute the comforting arm, the supportive ally, and the understanding listener that we often seek. It's like the shadow that never leaves you, always there, in every step of your journey. Coming to the story from my life, having dealt with disabilities in the past, I had hit a rough patch where everything seemed gloomy. Here I was, in the beautiful city of Melbourne, with my loyal companion Molly by my side, yet struggling with intense emotions.
That's when I decided to seek therapy. Initially, I was skeptical about this whole 'talk about your feelings' stuff. But, just like a hesitant cat venturing towards an unfamiliar box, I tip-toed into the world of therapy. It was here that I was able to unfold my narrative, align my emotions, and navigate my life with a new perception. It taught me to reconstruct my thoughts, not dismiss them. It offered me the space to acknowledge, cherish, and nurture my mind-body connection, enhancing my overall well-being. After all, isn’t life all about turning the mess into a beautiful message?
To wrap it up, managing proctitis is more than just dietary changes and medications. It's about embracing the power of talking, cultivating the mind-body connection, transforming your perception, and seeking support. And who knows, you might just turn your ordeal into a fascinating tale to tell, just like I did.
Vanessa Guimarães
Oh sure, because talking about your rear end will magically cure the inflammation.
Lee Llewellyn
While many clamor about the mystical powers of conversation, the reality is far more pedestrian, and yet the enthusiasm for a quick fix remains astonishingly naive.
The inflammatory cascade in proctitis is driven by cytokines, immune cells, and vascular responses, which no amount of verbal venting can directly neutralize.
What does therapy actually modify are the stress hormones, such as cortisol, that can exacerbate the permeability of the mucosal lining, a nuance few laypeople grasp.
Furthermore, cognitive-behavioral frameworks have been empirically shown to reduce the perception of pain by reconditioning maladaptive thought patterns, thereby indirectly influencing physiological outcomes.
One must also appreciate that the placebo effect, a well‑documented phenomenon, can be harnessed by any competent practitioner, but it is not a substitute for evidence‑based treatment.
The United States healthcare system, with its labyrinthine insurance structures, often incentivizes medication over psychotherapy, a policy choice that reflects deeper ideological currents rather than patient welfare.
In contrast, countries with universal coverage tend to integrate mental health services early, yielding better adherence and lower complication rates for chronic gastrointestinal disorders.
To be blunt, suggesting that simply talking will eradicate bleeding and urgency is tantamount to culinary advice that a soufflé will rise without proper heat.
Nevertheless, the stress‑reduction component of therapy can lower sympathetic tone, which in turn may diminish vasoconstriction and improve mucosal blood flow-a plausible, though modest, benefit.
Patients who engage in mindfulness meditation often report a subjective sense of control, which can translate into better dietary compliance and timely medical consultations.
It is also worth noting that therapist‑patient rapport fosters accountability, encouraging individuals to adhere to prescribed anti‑inflammatory regimens.
From a neurobiological perspective, the prefrontal cortex modulates the autonomic nervous system, and therapy can strengthen this top‑down regulation, offering a subtle yet measurable impact on gut inflammation.
Admittedly, the magnitude of this effect varies widely among individuals, and it should never be presented as a panacea.
In the end, the most prudent approach is a multimodal strategy: pharmacotherapy, dietary modifications, and a calibrated psychosocial intervention.
Anything less is a romanticized oversimplification that does a disservice to patients seeking realistic relief.
So, while the author’s enthusiasm is commendable, the claim that therapy alone is the unsung superhero needs to be tempered with scientific rigor.
Drew Chislett
Therapy can act like a gentle reset button for the nervous system, giving you space to notice the body’s signals before they turn into full‑blown flare‑ups.
When stress drops, the gut’s barrier often repairs itself faster, so the combination of talking and a solid treatment plan can really move the needle.
Rosalee Lance
Consider the mind‑body connection as a dialogue rather than a monologue; the body whispers, the mind interprets, and together they can rewrite the narrative of suffering.
By reframing proctitis not as a curse but as a signal inviting deeper self‑inquiry, we start to dissolve the anger that fuels inflammation.
It is a quiet rebellion against the stigma that shackles us, a philosophical stance that transforms discomfort into a path of empowerment.
Such a stance, when voiced in a therapeutic setting, can reshape perception and, consequently, physiological response.
Kara Lippa
That perspective encourages a balanced outlook while keeping the conversation grounded.
Puneet Kumar
In many South Asian contexts, therapy is woven with cultural concepts like "sattva" and holistic wellbeing, which align nicely with evidence‑based stress reduction techniques.
When patients adopt mindfulness alongside dietary adjustments-such as incorporating turmeric and fermented foods-the synergistic effect can modestly attenuate inflammatory markers.
Healthcare providers should therefore frame counseling as an integral component of a culturally resonant, multidisciplinary plan.
michael maynard
Honestly, the whole “talking cures everything” spiel feels like a covert operation to distract us from pharmaceutical profit motives.