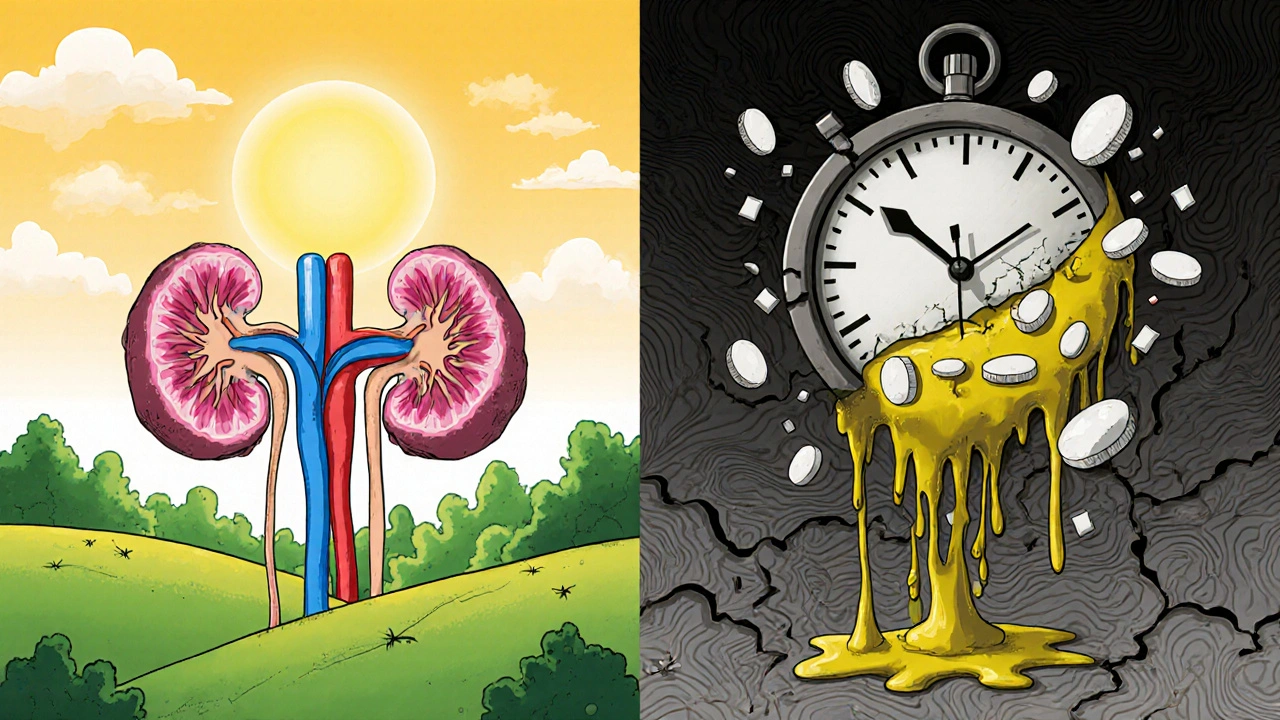
Most people don’t think about their kidneys until something goes wrong. But if you’ve started a new medication in the last few weeks or months and suddenly feel tired, have a fever, or notice you’re peeing less than usual, it could be something serious: acute interstitial nephritis. This isn’t just a minor side effect. It’s kidney inflammation triggered by drugs - and it’s more common than you think.
What Exactly Is Acute Interstitial Nephritis?
Acute interstitial nephritis (AIN) happens when the spaces between the tiny tubes in your kidneys - the interstitium - become inflamed. These tubes are what filter waste and balance fluids in your body. When they swell, your kidneys can’t work properly. The result? A sudden drop in kidney function, sometimes called acute kidney injury.
Unlike infections or autoimmune diseases that can cause kidney inflammation, drug-induced AIN is the most common cause. In fact, about 1 in 5 people with unexplained kidney problems have it. And it’s not just old-school antibiotics. Today, the biggest culprits are everyday medications you might not even think twice about.
Which Medications Cause It?
Over 250 drugs have been linked to AIN. But three types stand out:
- Antibiotics - Especially penicillin, ampicillin, and fluoroquinolones like ciprofloxacin. These cause about 35-40% of cases. Symptoms often show up within 1 to 3 weeks of starting the drug.
- Proton pump inhibitors (PPIs) - Omeprazole, esomeprazole, pantoprazole. These are the most common cause now. People take them for heartburn, often for months. AIN can appear after 10 to 12 weeks - or even up to 6 months later.
- NSAIDs - Ibuprofen, naproxen, diclofenac. These are risky for older adults and people with other health problems. Chronic use over months can trigger AIN, and sometimes it causes heavy protein loss in urine.
Even newer drugs like immune checkpoint inhibitors (used in cancer treatment) are now known to cause AIN - and they often need stronger, longer treatments to reverse the damage.
What Are the Real Signs?
Here’s the problem: AIN doesn’t always look like what you’d expect. Many people assume a rash, fever, and high eosinophils mean AIN. But those classic signs - called the hypersensitivity triad - show up in fewer than 10% of cases.
More common signs include:
- Less urine output (about half of patients notice this)
- Unexplained fatigue or nausea
- Swelling in the legs or ankles
- Fever (even mild)
- Flank pain (just below the ribs, on one or both sides)
Some people feel fine until a routine blood test shows their creatinine is up. That’s when doctors realize the kidneys are struggling. And because the symptoms are vague, AIN is often mistaken for a urinary tract infection, dehydration, or even the flu.
How Is It Diagnosed?
If your doctor suspects AIN, they’ll start with a urine test. Look for:
- Sterile pyuria - white blood cells in the urine, but no bacteria (70-90% of cases)
- Eosinophiluria - eosinophils (a type of immune cell) in the urine (30-70% of cases)
- Mild protein in the urine - usually under 2 grams per day, but NSAID cases can push past 3 grams
But urine tests alone aren’t enough. Blood tests will show rising creatinine - usually an increase of 0.3 mg/dL or more in 48 hours. If you’re over 65 or on multiple medications, this should raise a red flag.
The only way to confirm AIN is with a kidney biopsy. It shows immune cells swelling the spaces between kidney tubules, and often shows tubulitis - immune cells attacking the tubules themselves. Biopsies are most accurate when done within 3 to 7 days of symptoms starting.

Why Is This So Dangerous?
Left untreated, AIN can lead to permanent kidney damage. About 15-25% of people who don’t get help end up with chronic kidney disease or even need dialysis. Even when it’s caught early, many patients never fully recover their original kidney function.
Studies show younger people (under 50) usually bounce back in 6 to 8 weeks. But for those over 65, recovery can take 12 to 16 weeks - and some never get back to normal. One patient in Melbourne, 72, took omeprazole for heartburn for 4 months. When his creatinine spiked, he was told it was “just aging.” Three months later, his kidney function dropped to 30%. He needed steroids and months of monitoring. He’s at 65% now - but he’ll always need checkups.
What Should You Do If You Suspect AIN?
Time matters. The sooner you stop the drug, the better your chances.
- Stop the medication - If you’ve started a new drug in the last 3 months and have symptoms, talk to your doctor immediately. Don’t wait. Even if it’s an over-the-counter pill like ibuprofen or omeprazole.
- Get a kidney check - Ask for serum creatinine and urine tests. If results are unclear, push for a biopsy.
- See a nephrologist - Within 24 to 48 hours. This isn’t something a GP can manage alone.
- Don’t assume it’s a UTI - If you’re told you have a “bladder infection” but no bacteria show up in the urine, question it. That’s a red flag for AIN.
Some doctors prescribe steroids like prednisone to calm the inflammation. But here’s the catch: there’s no solid proof they work. Some nephrologists use them routinely. Others wait to see if kidneys recover on their own. The European guidelines say to use steroids if kidney function hasn’t improved after 7 days. The American guidelines are stricter - only for creatinine above 3.0 mg/dL.
Who’s at Highest Risk?
It’s not random. Certain people are much more likely to get AIN:
- People over 65 - They make up 65% of cases, even though they’re only 16% of the population.
- Those on 5 or more medications - This increases risk nearly 5 times.
- Women - They’re 1.8 times more likely than men to develop it.
- People with existing kidney issues or diabetes - Their kidneys are already under stress.
And here’s something most people don’t realize: many cases involve over-the-counter drugs. Patients often don’t tell their doctors about ibuprofen, naproxen, or antacids they’ve been taking daily. That’s why 40% of AIN cases have incomplete medication histories.
What’s Changing in the Field?
Research is moving fast. New blood and urine biomarkers like NGAL can detect AIN earlier than creatinine - with over 85% accuracy. AI tools are being trained to spot patterns in electronic records: if someone’s been on PPIs for 3 months and their creatinine starts creeping up, the system flags it before the doctor even sees the lab result.
Genetics may soon play a role too. Scientists found a gene variant - HLA-DRB1*03:01 - that makes people 4 times more likely to get AIN from PPIs. In the future, a simple genetic test might tell you if you’re at higher risk before you even start a new drug.
But right now, the best tool is awareness. The FDA updated PPI labels in 2021 to warn about kidney inflammation. The European Medicines Agency now requires special monitoring for cancer drugs linked to AIN. And in Australia, nephrologists are pushing for better education in primary care - because too many cases are missed until it’s too late.
What Happens After Recovery?
Even if your kidneys bounce back, you’re not out of the woods. Studies show most people have some lasting damage - even if it’s mild. That means:
- You’ll need regular kidney function tests (creatinine, eGFR) every 3 to 6 months
- You should avoid the drug that caused the problem - forever
- You should be cautious with NSAIDs, PPIs, and antibiotics in the future
- Keep a list of all your medications and share it with every new doctor
One nurse practitioner in Sydney told me she’s seen five cases in ten years. Three of them had permanent damage - even though they stopped the drug quickly. “It’s not just about the kidneys,” she said. “It’s about changing how you live after this.”
Final Thought: Don’t Ignore Subtle Changes
If you’ve started a new medication - even something as simple as a daily antacid - and you feel off, don’t brush it off. Fatigue, less urine, swelling, fever… these aren’t normal. They’re signals.
Acute interstitial nephritis is preventable. But only if you catch it early. The longer you wait, the harder it is to fix. And once your kidneys are damaged, you can’t get them back fully.
Know your meds. Know your body. And if something feels wrong - speak up.
Can over-the-counter painkillers cause kidney inflammation?
Yes. NSAIDs like ibuprofen and naproxen are a leading cause of medication-induced acute interstitial nephritis, especially in people over 50 or those taking them daily for months. Even though they’re available without a prescription, they can trigger serious kidney inflammation. If you’ve been using them long-term and notice swelling, less urine, or fatigue, get your kidney function checked.
How long does it take for AIN to develop after starting a drug?
It varies by drug. Antibiotics usually cause symptoms within 1 to 3 weeks. Proton pump inhibitors (like omeprazole) often take 10 to 12 weeks - sometimes up to 6 months. NSAIDs typically require months of daily use before AIN appears. If you’ve been on a new medication for more than a month and feel unwell, don’t assume it’s unrelated.
Is a kidney biopsy always necessary to diagnose AIN?
Not always, but it’s the only way to be sure. Urine and blood tests can strongly suggest AIN - especially if you have sterile pyuria and rising creatinine after starting a new drug. But if the diagnosis is unclear, or if your kidney function doesn’t improve after stopping the drug, a biopsy is needed. Delaying it past 7 days can make it harder to confirm the diagnosis.
Can you recover fully from medication-induced AIN?
Many people do - especially if the drug is stopped early and they’re under 50. Recovery rates are 80-90% for antibiotic-induced cases. But for PPIs and NSAIDs, full recovery is less common (60-70%). Most patients have some permanent loss of kidney function, even if they feel fine. Long-term monitoring is essential.
Should I take steroids if I have AIN?
It’s not clear-cut. Some doctors prescribe steroids like prednisone to reduce inflammation, especially if kidney function hasn’t improved after stopping the drug. But there’s no large study proving they work. European guidelines recommend them after 7 days of no improvement. American guidelines are more cautious - only for severe cases with creatinine above 3.0 mg/dL. Talk to a nephrologist about your specific situation.
Can AIN come back after recovery?
If you’re exposed to the same drug again, yes - and it can be worse. Once you’ve had drug-induced AIN, you’re at high risk for a repeat episode. Avoid the medication that caused it for life. Also be cautious with similar drugs in the same class. For example, if omeprazole caused it, avoid all PPIs. If ampicillin triggered it, avoid other penicillins.
Is AIN more common in older adults?
Yes. People over 65 make up 65% of all cases, even though they’re only 16% of the population. This is because older adults are more likely to take multiple medications - especially PPIs and NSAIDs - and their kidneys are less able to handle stress. Polypharmacy (taking 5 or more drugs) increases risk nearly fivefold.
What should I ask my doctor if I’m worried about AIN?
Ask: “Could any of my medications be affecting my kidneys?” Show them your full list - including supplements and over-the-counter pills. Ask if your creatinine has changed recently. Ask if sterile pyuria or eosinophiluria was checked in your urine test. And if you’re not getting answers, ask for a referral to a nephrologist. Early action saves kidneys.

archana das
So many people take omeprazole like candy and never think twice. I saw my aunt go from fine to needing dialysis because she thought heartburn was just part of aging. It’s not. It’s your kidneys screaming. Stop ignoring small changes.
Asha Jijen
LOL so now ibuprofen is the new heroin? Chill. My grandma takes Advil daily and still hikes 5 miles. You’re all overreacting.
Gayle Jenkins
THIS. I’m a nurse and I’ve seen too many cases where people are told ‘it’s just dehydration’ or ‘you’re getting older’ when their kidneys are shutting down. If you’re on more than 3 meds and feel off-get tested. Don’t wait. Your kidneys don’t send warning labels.
reshmi mahi
Ohhh so now we’re blaming Big Pharma AND your grandma’s Tums? 🙄 Next they’ll say breathing causes kidney failure. I’m just here for the drama.
Kaleigh Scroger
Let me tell you about my cousin who took naproxen for his arthritis for 8 months. No symptoms. No red flags. Then one day his creatinine jumped to 2.8. Biopsy confirmed AIN. He didn’t even know what that meant. He’s 54. Now he’s on a 10-year monitoring plan. And here’s the kicker-he never told his doctor he was taking it daily because he thought OTC meant ‘safe’. That’s the problem. We treat OTC like candy. It’s not. It’s pharmacology with a smiley face. And doctors? They don’t ask enough. They assume you’re telling them everything. You’re not. You forget the melatonin. You forget the turmeric capsules. You forget the 3 different antacids you’ve been stacking since 2021. We need better systems. Not just awareness. Systems. Like automated alerts in EHRs when someone’s been on PPIs for 90+ days with rising creatinine. AI can do this. But no one’s implemented it. Because paperwork. Because time. Because profit margins. And people die quietly while we argue about whether steroids work.
Emma Dovener
Just want to add-women over 65 on multiple meds are at the highest risk. And yes, it’s underdiagnosed because symptoms are vague. But if you’re tired, swollen, and your urine output dropped-don’t wait for a fever or rash. Those are rare. Go straight to a nephrologist. Don’t let your PCP brush it off. You’re not being dramatic. You’re being smart.
Jauregui Goudy
Bro. I took ibuprofen for a month straight after my knee surgery. Felt fine. Then my creatinine was up. Turns out I had AIN. Stopped the drug. Got steroids. Now I’m fine. But I learned: OTC doesn’t mean harmless. It means ‘you’re on your own’. Don’t be dumb. Know your meds.
Sue Haskett
PLEASE, PLEASE, PLEASE-write down every single thing you take. Every. Single. Thing. Even the ‘natural’ supplements. Even the herbal teas. Even the antacids you take ‘just once in a while’. Keep a list. Bring it to every appointment. Even if you think it’s ‘not important’. It’s always important. Your kidneys don’t care if you think it’s ‘just a little’-they only care if it’s in your system. And they don’t scream until it’s too late. Please. Just write it down.
shawn monroe
NGAL biomarkers are game-changers. We’re already seeing 85%+ sensitivity in early detection. The problem? Labs don’t test for it routinely. Why? Cost. Reimbursement. Silos. We have the tech. We have the data. We just don’t have the infrastructure. And until we fix that, people are going to keep losing kidneys to preventable inflammation. This isn’t science fiction. It’s clinical reality. And it’s happening right now.
Leo Adi
In India, people take painkillers like water. No prescriptions. No checks. I’ve seen men in their 60s with creatinine at 5.0 and still taking diclofenac. They say ‘Doctor, I feel better’. But their kidneys? Gone. We need community education. Not just hospital posters. Real talk. In local languages. In villages. In markets. This isn’t just a Western problem. It’s a human problem.
laura lauraa
How tragic. That someone would be so irresponsible as to ingest pharmaceuticals without consulting a licensed physician who has a PhD in nephrology and has read every single journal article since 1972. Truly, the ignorance of the masses is a cosmic tragedy. I weep for the kidneys. And for the poor, misguided souls who think ‘OTC’ means ‘unregulated chaos’.
Elizabeth Choi
Correlation isn’t causation. 40% of AIN cases have incomplete med histories-so maybe people just don’t remember. Maybe they’re lying. Maybe it’s coincidence. Also, biopsy is invasive. Why not wait? Maybe it’s just dehydration.
Emma louise
So now we’re blaming the American healthcare system for people being dumb? Wow. Maybe if you didn’t take every pill you saw on TV, you wouldn’t have kidney problems. Also, I’ve never heard of this ‘AIN’ thing. Probably made up by Big Pharma to sell more tests. I’ve been on omeprazole for 10 years. I’m fine. Your kidneys are weak. Not the drugs.
Tom Shepherd
wait so if i took ibuprofen for a week and now i feel tired is it ainn or just me being lazy
Allison Turner
Another fear-mongering post. People are dying from stress over this. Just stop taking meds if you’re scared. Or better yet-don’t read medical blogs. Go outside. Breathe. Your kidneys will thank you.