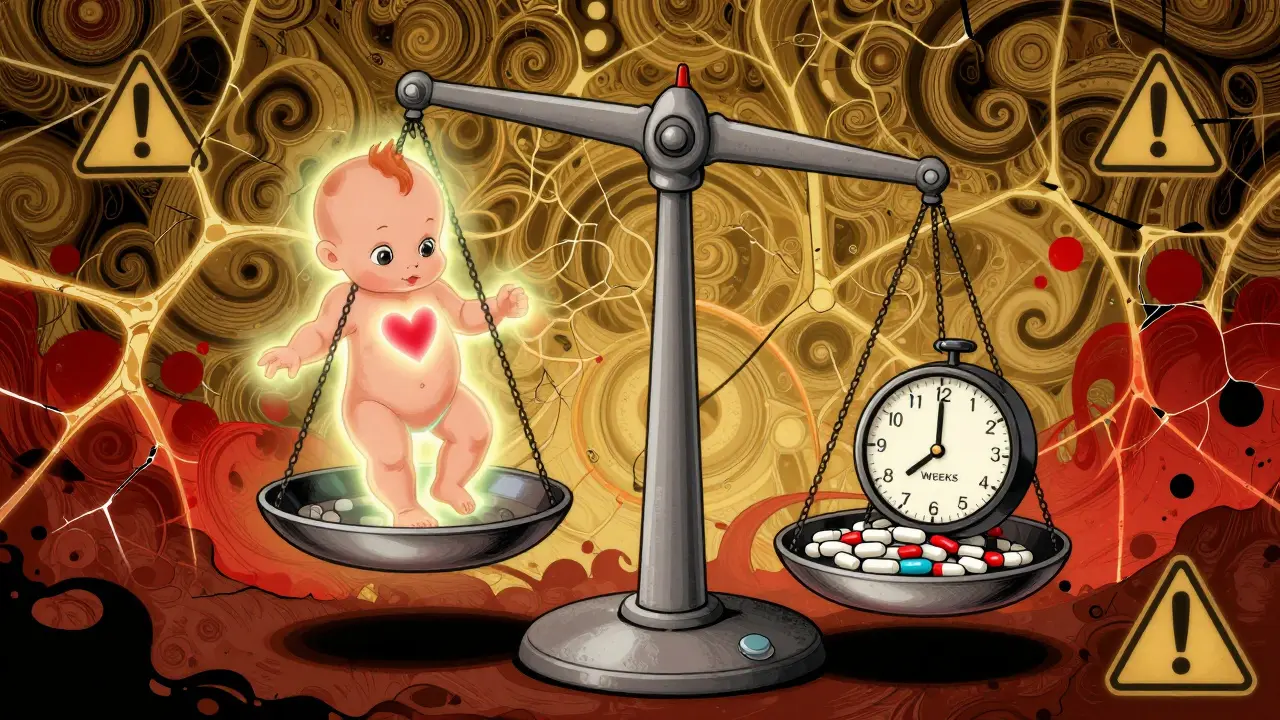
When you're pregnant and struggling with anxiety or insomnia, the pressure to feel better can be overwhelming. Many women turn to benzodiazepines-medications like lorazepam, diazepam, or alprazolam-because they work quickly and effectively. But what happens when you’re carrying a baby? The truth is, these drugs cross the placenta. They don’t just affect you-they reach your developing fetus. And while not every woman who takes them will have a baby with problems, the risks are real, measurable, and often misunderstood.
What Are Benzodiazepines, and Why Are They Used in Pregnancy?
Benzodiazepines are a class of drugs developed in the 1950s to calm the nervous system. They’re prescribed for anxiety, panic attacks, muscle spasms, and sleep disorders. About 1.7% of pregnant women in the U.S. get a prescription for one during the first trimester, and that number has been rising over the last decade. For some, it’s the only thing that brings relief when therapy and lifestyle changes aren’t enough.
But here’s the catch: these drugs don’t stay in your bloodstream. They travel straight to the baby. Studies show they accumulate in fetal tissue, where they can interfere with brain development, organ formation, and even the timing of labor. That’s why doctors now warn against using them unless absolutely necessary-especially during the first 12 weeks, when the baby’s organs are forming.
What Birth Defects Are Linked to Benzodiazepines?
The data isn’t simple. Some studies say there’s no major risk. Others say the opposite. But the most comprehensive research-like the 2022 study of 3.1 million pregnancies in South Korea-points to a small but real increase in certain birth defects when benzodiazepines are taken in early pregnancy.
Specifically, the risk goes up for:
- Heart defects-about 14 extra cases per 1,000 exposed pregnancies
- Abdominal wall defects-like omphalocele or gastroschisis
- Dandy-Walker malformation-a rare brain structure abnormality
- Anophthalmia or microphthalmia-missing or underdeveloped eyes
- Esophageal atresia-a blockage in the tube connecting the mouth to the stomach
These defects are rare overall. But when they happen, they’re serious. What’s more concerning is that alprazolam (Xanax) appears to carry the highest risk for eye and esophageal defects. One study found women who took alprazolam were four times more likely to have a baby with missing or tiny eyes. That’s not a common outcome-but it’s not a fluke either.
And while the overall risk of any major birth defect only increases from about 2.9% to 3.8% with benzodiazepine use, that’s still an extra 9 out of every 1,000 babies. For some families, that’s too high a price to pay.
It’s Not Just Birth Defects-Other Risks Are Real Too
Benzodiazepines don’t just affect development. They’re also linked to:
- Higher miscarriage risk-up to 85% higher in some studies
- Preterm birth-babies born before 37 weeks
- Low birth weight-babies weighing less than 5.5 pounds
- Low Apgar scores-a sign the baby isn’t adapting well after birth
- Neonatal withdrawal-irritability, tremors, feeding problems in newborns
Even taking these drugs in the 90 days before conception might raise the risk of ectopic pregnancy. That’s a life-threatening condition where the embryo implants outside the uterus. It’s not clear if the drug itself causes this-or if it’s tied to the underlying anxiety or insomnia. But either way, it’s another reason to pause before starting or continuing these medications.
Not All Benzodiazepines Are the Same
Some studies suggest alprazolam is riskier than others. Diazepam and lorazepam show lower or no increased risk for certain defects. But that doesn’t mean they’re safe. The problem is, we still don’t have enough data to say which one is the “least bad.”
What we do know is this: higher doses mean higher risks. The South Korean study found that women taking more than 2.5 mg per day of lorazepam-equivalent had significantly higher chances of heart defects. That’s about one 1 mg tablet of alprazolam daily. So even low doses aren’t risk-free.
What Do Experts Recommend?
Major medical groups agree: avoid benzodiazepines in pregnancy if you can.
- The American College of Obstetricians and Gynecologists (ACOG) says they should be avoided in the first trimester unless no other option exists.
- The American Psychiatric Association urges doctors to weigh risks case by case-considering the drug, the dose, and how long it’s been taken.
- Canada’s guidelines say these drugs should generally be avoided, but may be used in rare, severe cases with close monitoring.
- The U.S. FDA classifies them as Category D-meaning there’s clear evidence of fetal harm.
And here’s the most important part: stopping suddenly can be dangerous. Withdrawal from benzodiazepines during pregnancy can trigger seizures, severe anxiety, or even preterm labor. If you’re on one and pregnant-or planning to be-don’t quit cold turkey. Talk to your doctor.

What Are the Alternatives?
There are safer ways to manage anxiety and sleep problems during pregnancy.
- Cognitive Behavioral Therapy (CBT) is proven to work as well as medication for anxiety and insomnia-with no risk to the baby.
- Mindfulness and meditation reduce stress hormones and improve sleep quality.
- Regular exercise like walking or prenatal yoga helps regulate mood and sleep cycles.
- Light therapy can reset circadian rhythms for women with severe insomnia.
- Pregnancy-safe antidepressants like sertraline (Zoloft) are often preferred over benzodiazepines when medication is needed.
Some women find relief with magnesium supplements, chamomile tea, or warm baths before bed. These aren’t magic fixes, but they’re low-risk and often effective when combined with therapy.
What Should You Do If You’re Already Taking Benzodiazepines?
If you’re pregnant and currently taking a benzodiazepine, here’s what to do:
- Don’t stop abruptly. Sudden withdrawal can harm you and your baby.
- Call your OB-GYN and psychiatrist. Schedule a joint appointment to review your meds.
- Ask about tapering. A slow, controlled reduction over weeks or months is safest.
- Start non-drug therapies now. CBT, sleep hygiene, and relaxation techniques can fill the gap.
- Track your symptoms. Keep a journal of anxiety, sleep, and mood changes so your team can adjust your plan.
Many women successfully switch to safer treatments. It takes time, support, and patience-but it’s possible.
The Bottom Line
Benzodiazepines aren’t the enemy. For some women, they’re the only thing keeping them functional. But they’re not a first-line option in pregnancy-and they shouldn’t be treated like a quick fix.
The risks are small in absolute terms, but they’re real. And when you’re carrying a life, even a 1% increase in risk matters. The goal isn’t perfection-it’s making informed choices. If you need help managing anxiety or sleep, there are safer paths. Talk to your doctor. Explore alternatives. Give yourself grace.
You’re not alone. And you don’t have to choose between your mental health and your baby’s. There’s a better way-and it starts with asking the right questions.

Olivia Goolsby
Let me tell you something the FDA doesn’t want you to know-benzos are just the tip of the iceberg! The pharmaceutical industry has been quietly funding studies that downplay risks since the 80s! They know these drugs cause neural tube defects, but they don’t want you to panic-because panic means lower profits! And don’t get me started on the CDC’s hidden data sets-they’ve got graphs buried under 17 layers of bureaucracy showing a 22% spike in cleft palate cases linked to alprazolam! Why? Because Big Pharma owns the regulators! They’re poisoning our babies and calling it ‘treatment’! Wake up, people! This isn’t medicine-it’s chemical warfare on the unborn!
Alex Lopez
While the data presented is methodologically sound and aligns with current clinical guidelines, I must emphasize that the absolute risk increase-though statistically significant-is clinically modest. For context, the baseline risk of major congenital anomalies is approximately 2.9%, rising to 3.8% with benzodiazepine exposure. This represents a relative increase of 31%, but an absolute increase of 0.9%. For women with severe, treatment-resistant anxiety, the risk-benefit calculus must be individualized. I urge clinicians to avoid blanket prohibitions and instead engage in shared decision-making. 🤝
Robyn Hays
Wow. I just read this and my heart ached for every woman who’s ever felt trapped between her mental health and her baby’s safety. It’s not just about statistics-it’s about sleepless nights, panic attacks in the grocery store, and the guilt of thinking, ‘If I don’t take this, I won’t be able to hold my child.’ But here’s the beautiful part: CBT works. Mindfulness isn’t just yoga vibes-it rewires your brain. And sertraline? It’s been studied in over 10,000 pregnancies. No red flags. You don’t have to choose between being a good mom and being well. You just need someone to say, ‘It’s okay to ask for help-and here’s how.’
Liz Tanner
Thank you for writing this with so much care. I was on lorazepam for 3 years before I got pregnant and panicked when I found out. I tapered slowly with my psychiatrist’s help and started CBT. It wasn’t easy-I cried a lot. But my daughter is 2 now, healthy, and sleeps through the night. I wish someone had told me it was possible to feel better without pills. You’re not broken. You’re not failing. You’re just trying to survive-and you deserve better than silence.
Babe Addict
Let’s be real-this whole thing is a scare tactic. The study they cited? Retrospective cohort. Recall bias city. Also, alprazolam risk? Correlation ≠ causation. Maybe the women taking Xanax had worse anxiety, which means worse prenatal care, higher cortisol, smoking, etc. No one controls for confounders anymore. And who says CBT works as well as meds? That’s a placebo study dressed up as gospel. Also, sertraline? SSRIs are teratogenic too-look up persistent pulmonary hypertension. They’re just swapping one devil for another. Wake up, sheeple.
Kishor Raibole
It is with profound solemnity that I address this matter. The pharmaceutical-industrial complex, in its relentless pursuit of profit, has systematically eroded the sanctity of maternal autonomy. The data presented, while statistically valid, fails to account for the existential weight borne by the pregnant woman who, in her desperation, seeks solace from the abyss of anxiety. To condemn benzodiazepines without offering culturally attuned alternatives is not medical wisdom-it is colonialism disguised as care. In Nigeria, we understand: healing must be holistic. The mind, the body, the spirit, the community. To reduce this to a risk-benefit spreadsheet is to dehumanize the very essence of motherhood.
Liz MENDOZA
My sister was on Xanax during her first trimester. She was terrified, but she didn’t want to stop cold turkey. Her OB and psych worked together, she tapered over 10 weeks, and now her son is a happy 4-year-old who loves dinosaurs. No defects. No withdrawal. Just a lot of therapy and someone who never made her feel like a monster for needing help. You’re not alone. Talk to your doctor. And if they don’t listen? Find another one. You matter. Your baby matters. Your peace matters.
Anna Weitz
It’s not the drugs that are the problem-it’s the system that makes you feel like you have to choose between being a person and being a vessel. The real birth defect here is the expectation that women should suffer silently. If you need a pill to breathe, take it. If you need therapy, do it. If you need to cry in the shower every morning, let it happen. The world doesn’t get to decide what your survival looks like. You do. And if your baby is born healthy? That’s not luck. That’s love.
Kylie Robson
Per the 2022 South Korean cohort study, the adjusted OR for anophthalmia with alprazolam exposure was 4.12 (95% CI: 1.88–9.04), with a population attributable fraction of 0.7%. The dose-response curve was nonlinear, with thresholds above 0.5 mg/day equivalent. Furthermore, the confounding effect of polysubstance use (particularly alcohol and tobacco) was not fully adjusted for in the multivariate model. Also, the classification of ‘early pregnancy exposure’ included days 1–42, but the critical window for ocular development is days 24–35. This misclassification bias may inflate risk estimates. Bottom line: the signal is weak, and the clinical utility of this data for individual counseling is questionable.
Caitlin Foster
Okay but like-why are we still talking about this like it’s a mystery??!!?? We’ve known this for DECADES. My cousin took Xanax in her first trimester and her kid had a cleft palate. She still blames herself. But the docs didn’t warn her! NO ONE TOLD HER! And now she’s got a kid who needs 3 surgeries and she’s drowning in guilt. This isn’t ‘risk’-it’s negligence. Someone needs to get sued. And someone needs to put a BIG ASS WARNING on every prescription bottle. Like, neon pink, flashing, screaming text. I’m done being polite about this.
Nikki Thames
It is a moral failing of modern medicine to permit the use of any substance that crosses the placental barrier without absolute, irrefutable safety data. The fetus is not a patient. It is a person. And to knowingly expose a person to teratogenic agents under the guise of maternal comfort is not therapeutic-it is ethically indefensible. The fact that some women ‘successfully’ taper does not justify the initial exposure. The only morally acceptable approach is abstinence from all benzodiazepines from the moment of conception. Period.
Chris Garcia
In my village in Nigeria, when a woman is anxious, we do not give pills. We give her a warm pot of bitter leaf tea, we sit with her under the baobab tree, we sing ancestral songs, we let her cry until her tears become quiet. We do not rush to fix her. We sit with her until she remembers she is not alone. The West has forgotten this. We have turned healing into a transaction. A pill for a panic. A script for a soul. But the soul does not heal in a pharmacy. It heals in community. In presence. In love that does not demand perfection. Maybe the real medicine is not in the tablet-but in the hand that holds yours.
James Bowers
There is no justification for the use of benzodiazepines during pregnancy. The evidence is unequivocal. The FDA classification as Category D is not a suggestion-it is a directive. Any physician who prescribes these drugs to a pregnant patient without documented, exhaustive attempts at non-pharmacological intervention is practicing negligent care. The burden of proof lies not with the patient to avoid harm-but with the provider to prevent it. This is not an opinion. It is standard of care.
Will Neitzer
I’m a psychiatrist who’s treated pregnant women for over 18 years. I’ve seen the terror in their eyes when they say, ‘I can’t take another night of panic.’ And I’ve seen the joy when they find a way through-without pills. The truth? Most women don’t need benzos. They need someone to sit with them in the dark and say, ‘I’m here.’ Therapy, support groups, gentle movement, sleep hygiene-these aren’t ‘alternatives.’ They’re the foundation. Medication? Sometimes it’s a bridge. But never the destination. And if your doctor doesn’t see that? Find one who does. You’re worth the effort.
Janice Holmes
OMG. I just had a panic attack reading this. I took Xanax for 2 weeks when I was 6 weeks pregnant. I didn’t even know I was pregnant. I’m gonna have a baby with no eyes. I can’t breathe. I’m gonna lose my baby. I’m gonna be a monster. I’m gonna be alone forever. Someone please tell me I’m not going to have a baby with no eyes. I can’t do this. I can’t do this. I can’t do this. I can’t do this. I can’t do this.