Why Your Cough Won’t Go Away
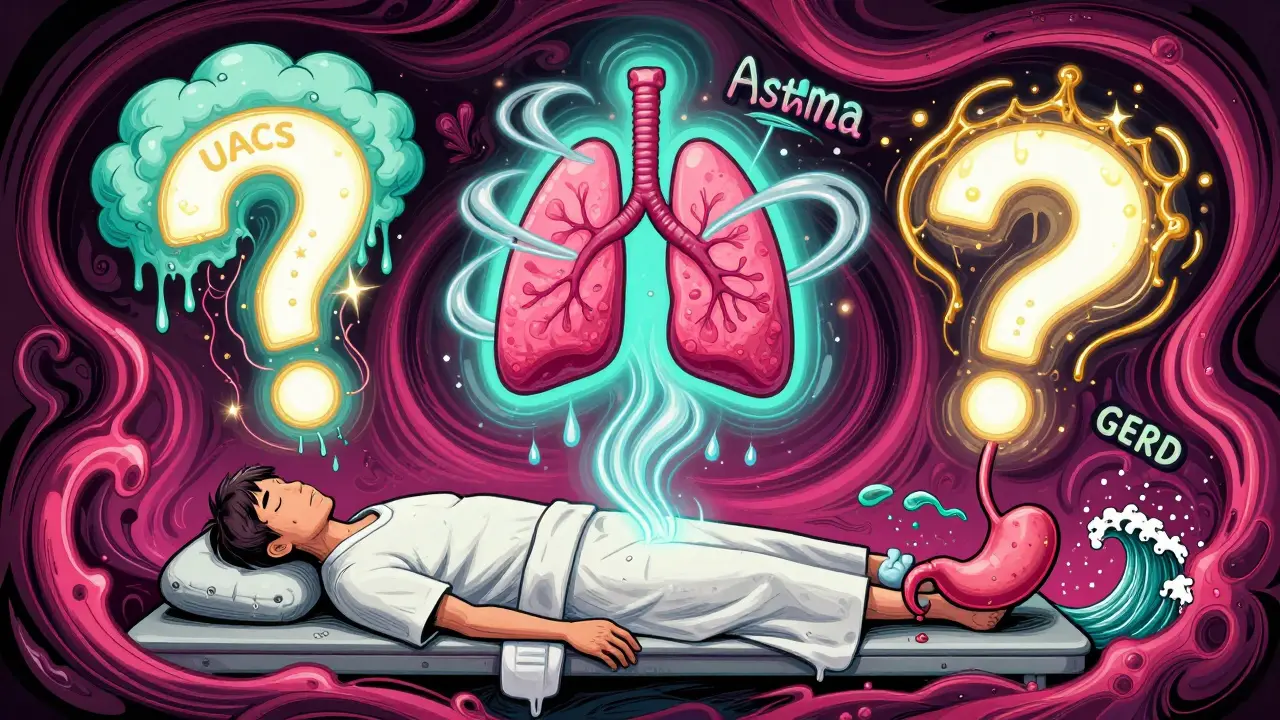
If you’ve been coughing for more than eight weeks, you’re not alone. About 1 in 10 adults deal with a chronic cough that doesn’t respond to over-the-counter remedies. And if you’ve already tried cough syrups, humidifiers, and even antibiotics, you’re probably frustrated. The truth? Most chronic coughs aren’t caused by colds or infections. They’re caused by three quiet, often overlooked conditions: GERD, asthma, and upper airway cough syndrome (formerly called postnasal drip).
These three issues together explain 80 to 95% of all chronic cough cases in people who don’t smoke or take ACE inhibitor blood pressure meds. That’s the first thing your doctor should check - not a CT scan, not a lung biopsy, not more antibiotics. Just these three.
The Three Big Causes - And How to Tell Them Apart
Let’s break them down one by one. Each has its own pattern, its own clues, and its own treatment path.
1. Upper Airway Cough Syndrome (UACS) - The “Postnasal Drip” Myth
Most people think of postnasal drip as mucus dripping down the back of the throat. But that’s not what’s really causing the cough. It’s the irritation of the nerves in your upper airway - triggered by inflammation from allergies, colds, or sinus issues. The cough isn’t from the mucus itself. It’s your throat’s overactive reflex.
This is the most common cause, responsible for 38 to 62% of chronic cough cases. The good news? It responds fast. If you take a first-generation antihistamine like diphenhydramine (Benadryl) plus a decongestant like pseudoephedrine for 2 to 3 weeks, and your cough improves? That’s your diagnosis.
Don’t use second-gen antihistamines like loratadine (Claritin) or cetirizine (Zyrtec). They don’t work as well for this. The older ones block histamine in the nerves that trigger cough. They also dry things up a bit, which helps. Side effects? Drowsiness. But that’s a small price if it stops the cough.
2. Asthma - The Silent Cough
Asthma doesn’t always mean wheezing or shortness of breath. In fact, about a quarter of adults with chronic cough have what’s called cough-variant asthma. Their only symptom? A dry, tickly cough - worse at night, after exercise, or when breathing cold air.
Here’s how to test for it: Your doctor will start with a simple breathing test called spirometry. If that’s normal, they might do a methacholine challenge. This test irritates your airways just enough to see if they overreact. A positive result means your airways are hypersensitive - a sign of asthma.
Response to treatment? If you use an inhaled corticosteroid (like fluticasone) for 4 to 8 weeks, and your cough fades? That’s your answer. No wheezing needed. Just a cough that disappears with asthma meds.
3. GERD - The Silent Reflux
GERD isn’t just heartburn. In fact, up to 70% of people with GERD-related cough have no burning sensation at all. It’s called “silent reflux.” Stomach acid creeps up into the throat and irritates the nerves that control coughing. You might notice it more after meals, when lying down, or after eating spicy food, chocolate, or coffee.
Diagnosing it used to mean swallowing a tube to measure acid in your esophagus. Now, guidelines say: skip the test. Start with a 4- to 8-week trial of a high-dose proton pump inhibitor (PPI) like omeprazole 40mg twice daily. If your cough improves? You’ve got GERD.
But here’s the catch: only 50 to 75% of people respond. And placebo works in about 40% of cases. That’s why some doctors now recommend using the Hull Airway Reflux Questionnaire (HARQ). A score above 13 strongly suggests reflux is the trigger. It’s faster, cheaper, and just as accurate.
What Your Doctor Should Do First
Before chasing down GERD, asthma, or UACS, your doctor needs to rule out the dangerous stuff. That means checking for:
- Weight loss without trying
- Coughing up blood
- Fever that won’t go away
- Swollen lymph nodes
- Abnormal sounds in your lungs on exam
If any of these are present, you need imaging - a chest X-ray at minimum. A normal X-ray rules out lung cancer, tuberculosis, or bronchiectasis in most cases. Don’t jump straight to a CT scan. The radiation isn’t worth it when the chance of finding cancer is less than 0.1% if your X-ray is clear.
Next, review your meds. Are you on an ACE inhibitor? Drugs like lisinopril or enalapril cause cough in 5 to 35% of users. It can start weeks or months after you begin taking them. If you are, ask your doctor if you can switch to an ARB like losartan. Cough often clears up in days to weeks.
Then comes the minimum workup: chest X-ray, spirometry, and a detailed history. That’s it. No need for allergy tests, CT scans, or expensive reflux monitors - yet.
Why the “Trial-and-Error” Approach Works
You might hear: “Why not just test for everything at once?” The answer is simple: it’s not cost-effective, and it doesn’t work better.
Each of the three conditions responds best to a targeted trial. UACS? Antihistamine + decongestant. Asthma? Inhaled steroid. GERD? High-dose PPI. If you try them all at once, you won’t know which one helped - or if it was just luck.
Doctors now treat them in sequence, not all at once. Why? Because UACS and asthma respond faster and more reliably. Start with UACS. If no improvement after 2 weeks, move to asthma. If still no luck, try GERD. Most people get relief within 6 to 8 weeks.
And if none of them work? That’s when you dig deeper. Could it be chronic refractory cough? Or something rare like vocal cord dysfunction or aspiration? But that’s the exception - not the rule.
What Doesn’t Work (And Why You’re Probably Wasting Time)
Let’s clear up some myths.
- Antibiotics? Only 1 to 5% of chronic coughs are from bacterial infections like pertussis. And even then, you need a special nasal swab - not a quick test. Most antibiotics do nothing.
- Over-the-counter cough syrups? They suppress the cough reflex temporarily, but they don’t fix the cause. And many contain dextromethorphan, which can make things worse by drying out your throat.
- Steam inhalation or honey? These might soothe your throat, but they won’t fix GERD, asthma, or UACS. They’re comfort, not cure.
- Ignoring your meds? If you’re on an ACE inhibitor and you’ve had a cough for months, that’s the culprit. Switching meds is the fastest fix.
Also, don’t wait for “classic” symptoms. You don’t need heartburn to have GERD-related cough. You don’t need wheezing to have asthma. You don’t need a runny nose to have UACS. The cough is the only symptom - and that’s enough.
What to Do Next
If you’ve had a cough longer than 8 weeks:
- Write down when it started, what makes it worse, and what helps.
- Check if you’re on any ACE inhibitor meds (lisinopril, enalapril, ramipril, etc.).
- Ask your doctor for a chest X-ray and spirometry.
- Ask about trying a first-gen antihistamine (like diphenhydramine) with pseudoephedrine for 2 weeks.
- If no change, ask about an inhaled steroid for 4 to 8 weeks.
- If still no improvement, ask about a high-dose PPI (omeprazole 40mg twice daily) for 4 to 8 weeks.
Keep a simple log: rate your cough on a scale of 1 to 10 each day. Note any triggers - food, weather, lying down. This helps your doctor see patterns.
What’s New in 2026
The field is changing. The term “postnasal drip” is being replaced with “upper airway cough syndrome” because it better reflects the nerve sensitivity involved. The Hull Cough Questionnaire is now the gold standard for measuring how much your cough affects your life.
And new drugs are coming. Gefapixant, approved in late 2022, reduces cough frequency by nearly 20% in people who don’t respond to standard treatments. Another drug, camlipixant, showed even better results in early 2024 trials. These aren’t cures, but they’re hope for the 10 to 20% who’ve been told, “We don’t know why you’re coughing.”
Even AI is stepping in. A 2023 study showed algorithms can analyze cough sounds and tell apart asthma-related cough from GERD-related cough with 87% accuracy. It’s not in clinics yet - but it’s coming.
For now, stick with the basics. The old rules still work. 80% of chronic coughs? Still caused by the same three things. The difference now? We know how to find them faster - and treat them better.
Can GERD cause a cough without heartburn?
Yes. Up to 70% of people with GERD-related cough have no heartburn or acid taste. This is called "silent reflux." The acid doesn’t need to reach the stomach - even small amounts that reach the throat can trigger coughing through nerve irritation. A high-dose PPI trial is still the best way to test for it.
Does asthma always cause wheezing?
No. About one in four adults with asthma only have a chronic cough - no wheezing, no shortness of breath. This is called cough-variant asthma. It responds to inhaled corticosteroids just like classic asthma. If your cough improves after 4 to 8 weeks of an inhaler, it’s likely asthma - even if you never wheeze.
Why do antihistamines help postnasal drip cough?
Not all antihistamines work the same. First-generation ones like diphenhydramine cross into the brain and block histamine receptors in the nerves that trigger cough. They also dry up mucus. Second-generation antihistamines like Zyrtec or Claritin don’t do this - so they’re much less effective for cough. That’s why older, sleepier antihistamines are still the go-to.
How long should I wait before seeing a doctor for a cough?
If your cough lasts more than 8 weeks, it’s time. Don’t wait for it to get worse. If you’re coughing for more than 3 weeks and it’s getting worse, or you have red flags like weight loss, fever, or coughing blood - see a doctor immediately. Chronic cough isn’t normal, even if you think it’s "just allergies."
Can I just take a PPI for my cough without testing?
It’s not recommended anymore. While PPIs help some people, up to 40% of people get better on placebo alone. That means if you take a PPI without a proper history and workup, you might think it worked - but it didn’t. Doctors now use questionnaires like HARQ or try UACS and asthma first. PPIs are the last step in the sequence, not the first.
Bob Cohen
I used to think my cough was just allergies until I tried Benadryl + pseudoephedrine for two weeks. Boom. Gone. Why do doctors still make you do 10 tests before trying the cheapest, most effective fix?
Also, ACE inhibitors? Yeah, I was on lisinopril for 8 months and didn’t connect the dots. Switched to losartan - cough vanished in 5 days. Why isn’t this the first question on every intake form?
Nidhi Rajpara
The article is extremely well-researched and scientifically accurate. However, I must point out that the term "silent reflux" is not universally accepted in all medical communities, particularly in South Asia, where diagnostic criteria may differ slightly due to dietary and environmental factors. Nonetheless, the protocol outlined here is commendable.
Lisa Rodriguez
OMG I’ve been coughing for 11 months and thought I was just sick all the time. I tried honey, steam, guaifenesin, everything. Then I read this and tried the diphenhydramine thing - like 3 days later I woke up and realized I hadn’t coughed once overnight. I’m crying. This is the first time in a year I slept through the night. Thank you for writing this.
Also, my doctor laughed when I asked about PPIs. Like, really? I’m not even sure he knew what HARQ was.
vivian papadatu
I work in pulmonology and this is spot on. The biggest mistake I see? People jumping straight to PPIs. I had a patient last month who’d been on omeprazole for 6 months - no improvement. Turns out she had cough-variant asthma. Started on fluticasone - cough gone in 10 days.
And yes, second-gen antihistamines are useless for this. I tell my patients: if you want to treat UACS, you need the sleepy ones. Drowsiness is the price of silence.
Deep Rank
I feel like everyone’s just repeating the same textbook stuff here. But have you considered that maybe your cough isn’t GERD or asthma at all? Maybe it’s anxiety? Or maybe you’re just stressed and your body is screaming for attention? I’ve seen so many people waste years on PPIs and inhalers when what they really need is therapy. Also, why do you trust doctors who don’t even know the difference between first-gen and second-gen antihistamines?
And what about your diet? Sugar, dairy, gluten - all inflammatory. Maybe you’re not coughing from reflux, you’re coughing from cheese. Just saying.
Chris & Kara Cutler
This saved my life. 💪
Rachel Liew
I’ve had this cough for 2 years and felt so alone. I didn’t know it could be from my blood pressure med. I switched to losartan last week and already feel lighter. Thank you for explaining it so clearly - I finally feel like someone gets it.
Jamie Allan Brown
I’m a GP in Scotland and I’ve been using this exact algorithm for years. The only thing I’d add: if you’re over 50 and smoke (even decades ago), do a chest X-ray before anything else. I had a patient who thought it was just "old man cough" - turned out it was early-stage lung cancer. X-ray caught it. No CT. No biopsy. Just a simple chest film. Sometimes the oldest tools are still the best.