More than 10% of people in the U.S. say they’re allergic to penicillin. But here’s the twist: up to 90% of them aren’t. That’s not a typo. Most people who think they’re allergic to penicillin have either outgrown it, misdiagnosed a side effect as an allergy, or were labeled allergic based on outdated or inaccurate testing. This misunderstanding doesn’t just cause confusion-it leads to worse health outcomes and higher costs. When doctors avoid penicillin because of a reported allergy, they often turn to broader-spectrum antibiotics. Those drugs cost about $500 more per hospital stay and increase the risk of resistant infections. The real problem isn’t the allergy itself-it’s the lack of proper evaluation.
What Really Counts as a Drug Allergy?
Not every bad reaction to a drug is an allergy. An allergy means your immune system mistakenly treats the drug as a threat. That triggers real immune responses: hives, swelling, trouble breathing, drop in blood pressure. These are immediate reactions, usually within an hour. That’s what counts as a true drug allergy. But a lot of people confuse side effects with allergies. Nausea from an antibiotic? That’s not an allergy. A headache after taking ibuprofen? Not an allergy. A rash that shows up days later? That might be a delayed reaction, which is different from IgE-mediated allergies. These distinctions matter because only true immediate-type allergies are candidates for desensitization. Penicillin is the most common drug allergy people report. But NSAIDs-like ibuprofen, naproxen, and aspirin-are close behind. People with NSAID allergies often react with hives, asthma flare-ups, or even anaphylaxis. Unlike penicillin, there’s no skin test for NSAID allergies. Diagnosis comes from a detailed history and sometimes a controlled challenge under supervision.How Penicillin Allergy Is Tested-and Why Most People Are Wrong
If you think you’re allergic to penicillin, the first step is skin testing. It’s simple: a tiny amount of penicillin and its breakdown products is placed under your skin. If you’re truly allergic, you’ll get a red, itchy bump. But here’s the catch: many clinics still use a substance called PPL (Prepared Penicillin Polylysine), which is outdated and unreliable. Up to 70% of people who react to PPL don’t react to actual penicillin. That’s why the American Academy of Allergy, Asthma & Immunology says PPL shouldn’t be used anymore. After a negative skin test, doctors often give a single full dose of amoxicillin-called a drug challenge. If you don’t react, you’re cleared. No more allergy label. No more unnecessary antibiotics. This step is the gold standard. Yet, too many patients skip it. They’re told, “You’re allergic. Don’t take penicillin,” and that’s the end of it. That’s not care. That’s assumption.NSAID Allergies: No Skin Test, But Still Manageable
Unlike penicillin, there’s no reliable skin test for NSAID allergies. So how do you know if you’re truly allergic? It comes down to your history. Did you break out in hives within an hour of taking aspirin? Did you have trouble breathing after taking ibuprofen? If yes, you likely have a true allergy. The good news? NSAID allergies can be managed with desensitization-especially for people who need these drugs long-term, like those with arthritis or heart disease. The process is different from penicillin. Instead of one-time, rapid dosing, NSAID desensitization often involves daily, slowly increasing doses. For example, starting at 30 mg of aspirin, then 60 mg, then 100 mg, and so on, until you reach your needed dose. Once you’re desensitized, you can keep taking it daily. The tolerance lasts as long as you keep taking the drug. This isn’t a cure. Stop taking it for a few days, and you might lose tolerance. But for people who rely on NSAIDs to function, this is life-changing.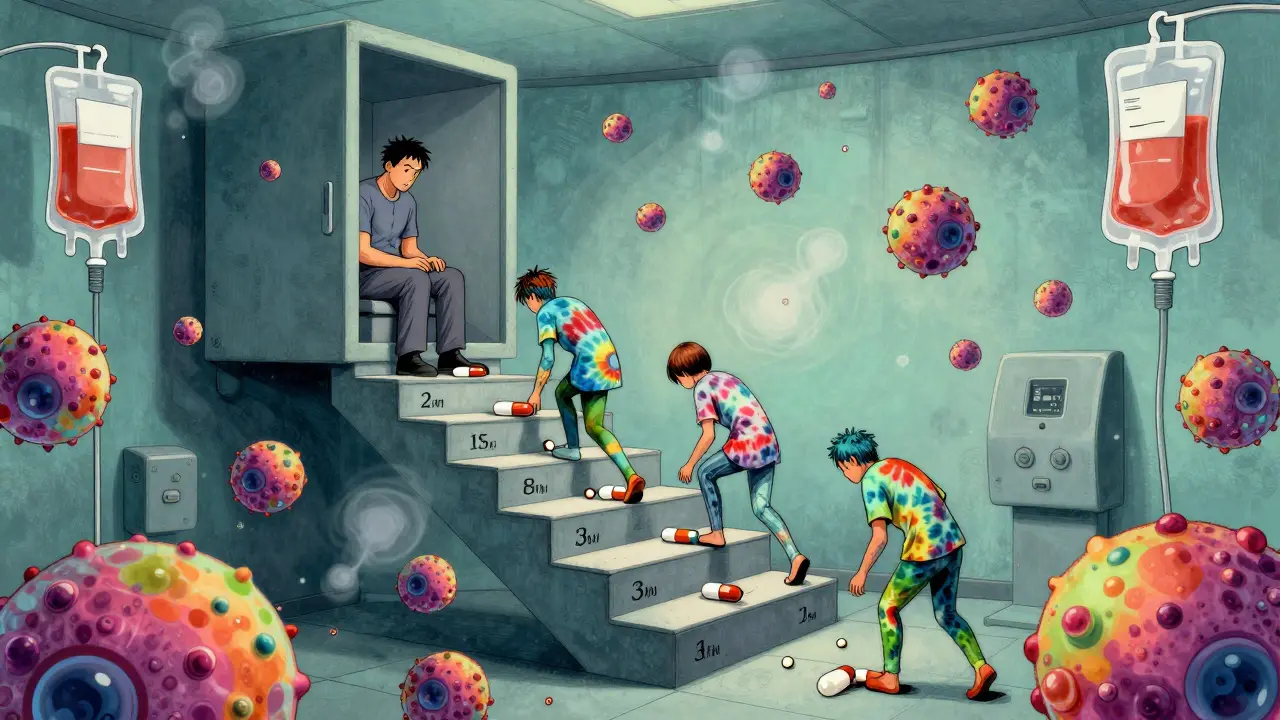
Desensitization: How It Works and When It’s Needed
Desensitization isn’t magic. It’s science. The idea is simple: expose the immune system to tiny, increasing amounts of the drug over hours. This doesn’t change your allergy-it temporarily tricks your body into ignoring it. Think of it like slowly walking into a cold pool. At first, it’s shocking. But if you go in bit by bit, your body adjusts. The most common protocol is the 12-step method. It starts with a dose that’s one-ten-thousandth of the full amount. Every 15 to 20 minutes, the dose doubles. By the end of 4 to 8 hours, you’ve reached your full therapeutic dose. Some protocols, especially for beta-lactam antibiotics like cefazolin or ceftriaxone, can be done in under two and a half hours by tripling the dose every 15 minutes. This only works if you’re getting the drug for one course of treatment. Need it again next month? You’ll need to go through it again. That’s why it’s not used for everyday medications like blood pressure pills. It’s reserved for critical cases: severe infections, cancer drugs like paclitaxel, or when no alternatives exist.Who Can Get Desensitized? And Who Can’t?
Not everyone is a candidate. You need two things: a confirmed immediate-type allergic reaction, and no safe alternative drug. If you can take another antibiotic, you won’t be desensitized to penicillin. If you have a mild rash from ibuprofen but can use acetaminophen, you won’t need desensitization. Severe reactions like anaphylaxis, laryngeal swelling, or uncontrolled low blood pressure make desensitization risky. If you’ve had a life-threatening reaction, your doctor will weigh the risks carefully. Some protocols require pre-treatment with antihistamines or steroids to reduce the chance of a reaction during the process. Children are a growing focus. Most protocols were designed for adults. But kids with cancer, chronic infections, or cystic fibrosis need these drugs too. Pediatric allergists are now working with oncologists and infectious disease specialists to adapt protocols. Still, there’s no universal pediatric guideline. That’s a gap.
Where and How Desensitization Is Done
This isn’t something you do at your local pharmacy. Desensitization must happen in a hospital or specialized allergy clinic with immediate access to emergency equipment: epinephrine, oxygen, IV fluids, and staff trained to handle anaphylaxis. The team includes allergists, nurses, and sometimes pharmacists who understand the exact dosing schedules. The route matters too. You might be desensitized through IV, but then switch to oral once you’re done. That’s common with antibiotics. The goal isn’t to give you the drug the same way every time-it’s to get you to the full dose safely, then let you continue therapy in the most practical way. And yes, things can go wrong. About 2% of people who’ve been desensitized to penicillin have a reaction again if they’re re-exposed later, especially after getting it through injection. That’s why some doctors recommend retesting with skin tests before giving penicillin again, particularly after a serious reaction.Why This Matters Beyond the Individual
When you’re labeled penicillin-allergic and you’re not, you’re not just stuck with a label. You’re part of a bigger problem: antibiotic resistance. Broader-spectrum antibiotics kill more good bacteria and push resistant strains to grow. Hospitals see more C. diff infections, longer stays, and higher costs-all because of mislabeled allergies. Correcting this saves money, saves lives, and reduces the burden on healthcare systems. But it takes action. Patients need to ask: “Was I tested properly?” Doctors need to offer skin testing and challenges. Clinics need to have desensitization protocols ready. Right now, only major academic hospitals have the infrastructure. But the need is growing. With more awareness, this could become standard care-not a last resort.What’s Next for Drug Allergy Management?
The field is moving fast. Accelerated protocols are becoming routine. More drugs are being added to the list of those that can be desensitized-like antifungals (fluconazole, voriconazole) and even some chemotherapy agents. Researchers are also exploring whether desensitization could work for non-IgE reactions, like delayed rashes or organ inflammation. That could open doors for people who were previously told, “There’s nothing we can do.” The big push now is standardization. Right now, every hospital has its own protocol. Some are 12 steps. Some are 8. Some use different concentrations. That’s dangerous. If a nurse isn’t trained on your hospital’s method, mistakes happen. International guidelines are being drafted, but they’re not yet mandatory. The future is clear: accurate diagnosis first. Desensitization when needed. Collaboration between allergists, infectious disease doctors, oncologists, and pediatric specialists. And for every person who thinks they’re allergic to penicillin-it’s time to get tested.Can I outgrow a penicillin allergy?
Yes. Many people outgrow penicillin allergies over time. Studies show that up to 80% of people who had a true reaction as a child lose their sensitivity after 10 years. But you shouldn’t assume you’re no longer allergic. The only way to know is through skin testing and a supervised drug challenge.
Is desensitization safe for children?
Yes, when done properly. Children with cancer, severe infections, or cystic fibrosis can benefit from desensitization. However, most protocols were designed for adults, so pediatric doses and schedules must be carefully adjusted. It should only be done in centers with experience in both allergy and pediatric care.
Can I do NSAID desensitization at home?
No. NSAID desensitization must be done under medical supervision. Even though it’s sometimes done daily over weeks, the first few doses carry a risk of reaction. Only trained staff in a facility with emergency equipment should manage this process.
What happens if I stop taking the drug after desensitization?
Your tolerance doesn’t last forever. If you stop taking the drug for more than a few days-usually 48 to 72 hours-you’ll lose the temporary protection. If you need the drug again, you’ll have to go through desensitization once more. That’s why it’s only used for short-term or repeated courses, not lifelong daily use unless you’re on a maintenance schedule.
Are there alternatives to desensitization for drug allergies?
Yes, but only if safe alternatives exist. For penicillin, other antibiotics like vancomycin or clindamycin can be used. For NSAIDs, acetaminophen or corticosteroids may work. But if you have a serious infection or cancer and those alternatives are less effective, more toxic, or not available, desensitization is often the only option to get life-saving treatment.

phara don
So wait-90% of people who think they’re allergic to penicillin aren’t? That’s wild. I’ve been avoiding it my whole life because my mom said I broke out as a kid. Guess I should get tested before my next infection… 🤔
Ellie Norris
OMG this is so important!! I had a rash after amoxicillin when I was 5 and was labeled allergic forever. Turned out it was just a viral rash. Got tested last year and now I can take penicillin again-saved me so much stress and money. Seriously, if you think you’re allergic, get tested!! 😊
Marc Durocher
Let me get this straight-we’re telling people to risk anaphylaxis just to save $500 per hospital stay? That’s not a cost-saving measure, that’s a gamble with lives. And don’t even get me started on how many docs just shrug and say ‘avoid penicillin’ without even trying to confirm. Lazy. Sad. And honestly? A little dangerous.
larry keenan
It is imperative to underscore the distinction between IgE-mediated hypersensitivity and non-allergic adverse drug reactions. The majority of reported penicillin allergies are misattributed to non-immunologic phenomena, such as gastrointestinal distress or delayed maculopapular eruptions. Consequently, the overutilization of broad-spectrum agents contributes significantly to antimicrobial resistance. Proper diagnostic protocols, including skin testing and graded challenge, remain underutilized in primary care settings.
Nick Flake
Imagine if we treated food allergies the same way we treat drug allergies. ‘Oh you had a stomachache after eating shrimp? Yeah, you’re allergic. Never eat seafood again.’ We’d be in chaos. But somehow, with drugs, we just slap a label on people and call it a day. It’s not just medical negligence-it’s a cultural failure. We’ve turned healthcare into a guessing game. And people are paying the price. 💔
Chinmoy Kumar
really cool info! i never knew NSAIDs could be desensitized. my grandpa has arthritis and he's been avoiding ibuprofen for years because he got a rash once. maybe he can try this? i'll tell him about it. thanks for sharing!!
Vatsal Srivastava
Penicillin allergy is overblown because doctors are lazy and hospitals want to bill for expensive antibiotics. Also, most people who say they're allergic are just bad at reading side effect pamphlets. You get diarrhea? Allergy. Headache? Allergy. Too much coffee? Allergy. Fix your life before blaming penicillin.
Brittany Marioni
Wait-so if you’re allergic to penicillin, but you’re not really allergic, and you get desensitized, and then you stop taking it for three days, you’re allergic again? So you have to do the whole process again? That’s insane. Who has time for that? And why isn’t this more widely available? Why is it only at ‘major academic hospitals’? This is ridiculous. We need this everywhere. Everywhere. Everywhere.
Akhona Myeki
Of course Americans think penicillin allergies are overdiagnosed-because you all overprescribe antibiotics like candy. In South Africa, we don’t have enough penicillin to go around. We don’t have the luxury of mislabeling allergies. We have people dying because they can’t get the right drug. So don’t lecture us about your ‘misdiagnosed’ allergies. Fix your broken system first.
clarissa sulio
My cousin was told she was allergic to penicillin as a baby and now she’s 32 and still avoids it. She got a bad UTI last year and had to take clindamycin for two weeks. Got C. diff. Now she’s on probiotics for life. If they’d just tested her, she’d have been fine. This isn’t just inconvenient-it’s life-changing.
Bridget Molokomme
So you’re telling me I could’ve had the cheap antibiotic instead of the $800 one last year… if I’d just asked for a skin test? I feel like an idiot. Also, why does this feel like a plot twist in a medical thriller?
Ansley Mayson
People are allergic to penicillin. End of story. Stop trying to fix what isn’t broken. If you don’t want to take the risk, don’t. Simple.