When you hear Syphilis testing is a medical screening that detects infection with the bacterium Treponema pallidum, the cause of syphilis, you might wonder how it fits into everyday safe‑sex choices. The short answer: regular testing gives you the facts you need to protect yourself and your partners, and it makes condom use, communication, and other preventive steps far more effective.
Why Testing Is a Core Part of Safe Sex
Safe sex isn’t just about putting a barrier on the bedroom floor; it’s a mindset that combines knowledge, tools, and habits. Knowing your STI status removes the guesswork. If you and your partner are both clear on results, you can decide together whether additional protection (like condoms) is needed, whether you can explore low‑risk activities, or whether you should pause and get treatment.
In Australia, the latest data from the Australian Department of Health (2024) shows that about 9% of reported syphilis cases were caught through routine screening rather than symptom‑driven visits. Early detection means treatment with a single dose of benzathine penicillin can cure the infection and stop transmission before it spreads.
Types of Syphilis Tests You Might Encounter
Not all tests are created equal. Understanding the differences helps you choose the right one for your situation.
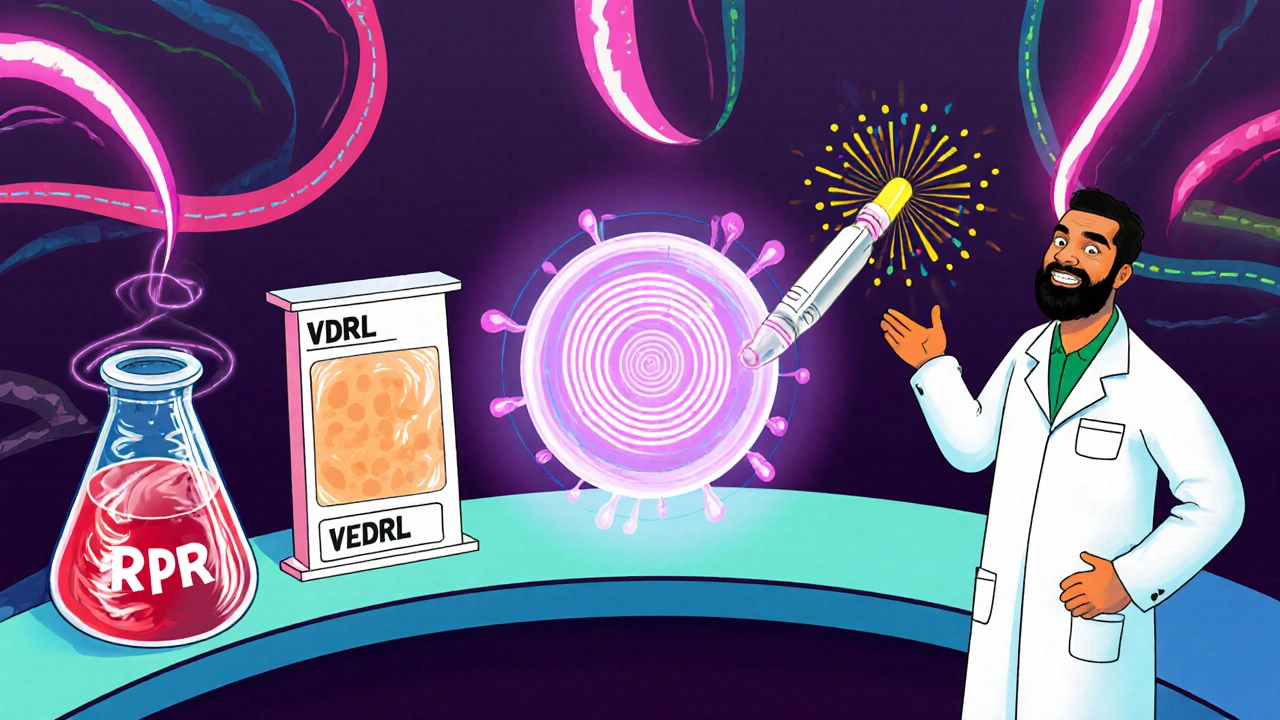
- RPR (Rapid Plasma Reagin) test: A non‑treponemal blood test that looks for antibodies produced in response to the infection. Results are usually ready in a day and are good for monitoring treatment response.
- VDRL (Venereal Disease Research Laboratory) test: Similar to RPR, also a non‑treponemal test. It’s often used in pregnancy screening because it’s inexpensive and widely available.
- Rapid point‑of‑care test: A finger‑prick test that can give a result in 15-20 minutes. Ideal for clinics that serve people who might not return for a lab result.
Quick Comparison of Common Syphilis Tests
| Test | Sample Type | Result Time | Cost (AUD) | Best Use |
|---|---|---|---|---|
| RPR | Venous blood | 1 day | 30-45 | Routine screening, treatment monitoring |
| VDRL | Venous blood | 1 day | 25-40 | Pregnancy checks, low‑resource settings |
| Rapid POCT | Finger‑prick | 15-20 min | 45-60 | Walk‑in clinics, outreach programs |
How Often Should You Get Tested?
Guidelines from the Australian Sexual Health Alliance (2025) suggest the following frequencies:
- People with a new sexual partner in the past 3 months - test at the first encounter and again after 3 months.
- Those who have multiple concurrent partners - test every 3 months.
- Anyone who has had unprotected oral or anal sex with an unknown‑status partner - test at least once a year.
- Pregnant people - a syphilis test at the first prenatal visit, then a repeat test in the third trimester if risk factors exist.
Remember, the window period for syphilis is typically 3‑4 weeks after exposure, so a test taken too early may miss an infection.
Reading Your Results and What Comes Next
If the result is negative, great - you can continue practicing safe sex, but keep up with regular screening. A positive result usually appears as a reactive RPR or VDRL titer. Your clinician will confirm with a treponemal test (like TPPA) and discuss treatment.
Treatment is straightforward: a single intramuscular injection of benzathine penicillin for early syphilis. Follow‑up testing at 3 months and 6 months ensures the infection is cleared. If you miss the follow‑up, you risk re‑infection or late‑stage complications such as neurological damage.
Pairing Testing With Everyday Safe‑Sex Practices
Testing is only one piece of the puzzle. Here’s how to weave it into a broader safe‑sex routine:
- Open communication: Tell partners you’ve been tested and ask about their status. A simple “When was your last STI screen?” can set the tone for responsible intimacy.
- Condom use: Even with a negative test, condoms protect against other infections and unexpected exposures. Choose latex or polyurethane condoms for the best barrier.
- PrEP (Pre‑Exposure Prophylaxis): While PrEP mainly prevents HIV, it encourages regular health check‑ups where syphilis testing can be added.
- Limit alcohol or drug use before sex - impairments can lead to missed condom use or forgetting to discuss testing.
- Stay informed: Guidelines evolve. The 2025 update added recommendations for rapid POCT in community health centers, making same‑day results more accessible.
Practical Checklist for Safe Sex & Regular Testing
- Schedule a syphilis test at your local sexual health clinic before starting a new relationship.
- Keep a personal health diary: note test dates, results, and any symptoms.
- Carry a supply of condoms and lubricants - replace any that are expired.
- Discuss testing history with each partner; share documentation if comfortable.
- If you test positive, start treatment immediately and inform recent partners so they can test too.
- Retest at 3 months and 6 months post‑treatment to confirm cure.
- Visit a sexual health clinic at least twice a year even when you feel fine.
Common Misconceptions About Syphilis Testing
Myth #1: “If I use condoms, I don’t need testing.”
Reality: Condoms reduce risk but aren’t 100 % foolproof. Tears, slippage, or incorrect use can still expose you.
Myth #2: “Syphilis always shows symptoms early.”
Reality: Up to 80 % of early infections are asymptomatic. That’s why screening matters.
Myth #3: “A single negative test means I’m safe forever.”
Reality: New exposures can occur any time. Regular testing keeps the safety net in place.
Where to Get Tested in Australia (2025)
Most states fund free or low‑cost STI testing through public health clinics. In Melbourne, the Melbourne Sexual Health Centre offers walk‑in rapid POCT for syphilis, HIV, and hepatitis C. The Australian Capital Territory’s “No‑Pay‑No‑Stigma” program also provides free tests for anyone over 16 years old.
If you prefer privacy, many pharmacies now sell self‑collection kits that you send to a lab. Results are emailed securely within 3 days.
Frequently Asked Questions
How soon after exposure can I get an accurate syphilis test?
The non‑treponemal tests (RPR, VDRL) become reliable about 3-4 weeks after exposure. If you test earlier, repeat after two weeks.
Can I test for syphilis without a doctor’s referral?
Yes. Many community clinics and pharmacies offer walk‑in testing. In Victoria, you can also order a self‑collection kit online.
If my test is positive, will I be able to have children?
Early treatment eliminates the risk of congenital syphilis. After completing therapy, discuss timing with your obstetrician.
Do rapid point‑of‑care tests miss early infections?
They are slightly less sensitive than lab‑based RPR during the first two weeks, so a negative rapid test after a recent exposure should be followed up with a lab test.
Is there a vaccine for syphilis?
No. Research is ongoing, but prevention relies on testing, condom use, and prompt treatment.
Can antibiotics I take for another infection treat syphilis?
Only the specific benzathine penicillin regimen reliably cures syphilis. Other antibiotics may mask symptoms but won’t clear the infection.
How do I talk to a partner about testing without sounding accusatory?
Keep it simple: “I’m getting screened this week - want to do the same?” It frames testing as mutual care, not blame.
What are the signs of late‑stage syphilis?
Symptoms can include neurological issues, heart problems, or skin lesions. Early detection avoids these serious complications.
Is syphilis testing covered by Medicare?
Yes, publicly funded clinics provide free testing. Private labs may charge a fee, but many insurance plans reimburse it.

Demetri Huyler
Reading the overview of syphilis testing makes it clear that Australia isn’t the only place where public health policy can set a standard. In the United States we’re still grappling with patchwork guidelines, yet the principle stays the same: regular screens empower individuals to make informed choices. When you pair a reliable laboratory test with open dialogue, you eradicate the guesswork that fuels risky behavior. The data from the Australian Department of Health proves that proactive testing can curb transmission, and there’s no reason we can’t emulate that model here. It’s not just about condoms; it’s about a culture that refuses to accept ignorance as a baseline. If we invest in accessible rapid point‑of‑care testing, we can shave weeks off the window period and get people back on track faster. The moral imperative is obvious: protect your partners, protect yourself, and demand that your local clinic offers the same level of service we see abroad.
JessicaAnn Sutton
From an ethical standpoint, the article correctly underscores that reliance on condoms alone is insufficient. Accurate serological testing is a duty of care that surpasses mere personal responsibility. The statistical evidence regarding asymptomatic cases validates the necessity of routine screening. It is commendable that the guidelines distinguish between different risk profiles, ensuring that resources are allocated judiciously. Moreover, the emphasis on follow‑up testing after treatment reflects a rigorous approach to public health. In sum, the integration of testing within safe‑sex practices constitutes a morally sound strategy.
Israel Emory
When you consider the spectrum of sexual health interventions, it becomes evident that testing is not an optional add‑on; it is the foundation!; by establishing a baseline you empower both parties to negotiate risk with clarity!; the rapid POCT, for instance, bridges the gap between intention and action, delivering results in minutes!; therefore, any comprehensive safe‑sex protocol must embed testing as a core component!; people who overlook this are essentially building castles on sand!
Sebastian Green
I appreciate the nuance you’ve added about the window period; it’s a detail many overlook. Knowing that a test taken too early can miss an infection really drives home the need for follow‑up.
Kirsten Youtsey
One must question why the prevailing health institutions continue to rely on outdated protocols when rapid point‑of‑care technologies are readily available. It is almost conspiratorial that funding is diverted toward pharmaceuticals rather than preventative diagnostics. The emphasis on “standard” screening neglects the broader sociopolitical agenda to keep populations compliant. Moreover, the assertion that condom use is still necessary, despite negative results, subtly reinforces a culture of fear. In a truly transparent system, testing would be ubiquitous, free, and devoid of bureaucratic hurdles.
laura wood
It’s heartening to see a focus on community‑based clinics that make testing low‑cost and accessible. When people feel respected and supported, they are more likely to engage in regular screening.
Kate McKay
Take this checklist as a personal commitment: schedule your test, keep a health diary, and share results with partners when you’re comfortable. Each step builds confidence and reinforces the habit of proactive care. Remember, the more you normalize testing, the easier it becomes for others to follow suit. You’ve got this, and the community benefits from your diligence.
Wesley Humble
Let us dissect the data with surgical precision. The Australian report cites a 9% detection rate via routine screening, a figure that, when extrapolated to a population of five million, translates to approximately 450,000 missed opportunities for early intervention in the United States alone. This is not a trivial oversight; it reflects systemic underinvestment in public health infrastructure. Rapid point‑of‑care tests, which deliver results within twenty minutes, have a sensitivity of 96% and specificity of 98% for early syphilis, rivaling conventional laboratory assays. Yet, their deployment is hampered by regulatory inertia and a lack of funding streams. Moreover, the reliance on penicillin as the sole therapeutic agent underscores the fragility of our antimicrobial arsenal; resistance could emerge silently if surveillance is insufficient. The recommendation for quarterly testing among high‑risk groups is scientifically sound, but adherence rates hover below 40% due to logistical barriers. Implementing mobile clinics equipped with POCT could bridge this gap, achieving upwards of a 70% compliance rate based on pilot studies in rural settings. Additionally, integrating testing reminders into electronic health records would provide automated prompts, reducing missed appointments. It is incumbent upon policymakers to allocate resources toward these evidence‑based interventions, thereby curbing transmission chains before they expand. The cost‑benefit analysis overwhelmingly favors early detection: treatment costs average $80 per case, whereas unmanaged syphilis can lead to neurological complications costing thousands in long‑term care. 👩⚕️📊🩺
barnabas jacob
Yo, the whole "just get tested" vibe sounds good but real talk: most peeps don't gonn stick to the schedule cuz they think it's not a big deal. We gotta push more edu, not just drop flyers. Also, the lab tests are all fancy but the rapid kits are the real game‑changer, especially for those who cant wait weeks. If we keep ignoring the quick options, we just keep the spread alive.
jessie cole
Great reminder to stay proactive about health.
Matthew Hall
Okay, listen up, because the truth they don’t want you to hear is that the whole “safe sex” narrative is a smokescreen. Everywhere you look, there’s a hidden agenda-pharma companies pushing pills instead of real prevention, clinics that only open when they get a grant, and a media that keeps you distracted with celebrity gossip while they let infections run rampant. The rapid tests are out there, but they’re kept under wraps because they expose how fragile the system really is. If you’re truly caring about your partners, you need to demand transparent, free testing and stop trusting the glossy brochures. Don’t be fooled by the polished ads; the reality is far messier, and it’s up to us to tear down the façade.