Every year, more than 23,000 people end up in the emergency room because a supplement they took messed with their medication. And here’s the scary part: most of them had no idea it could happen. You might think, It’s natural, so it’s safe. But that’s not true. A supplement labeled "herbal" or "organic" doesn’t mean it won’t interfere with your blood pressure pill, antidepressant, or heart medication. In fact, some of the most dangerous interactions come from things you can buy off the shelf at your local grocery store.
Why Supplements Can Be Just as Dangerous as Prescription Drugs
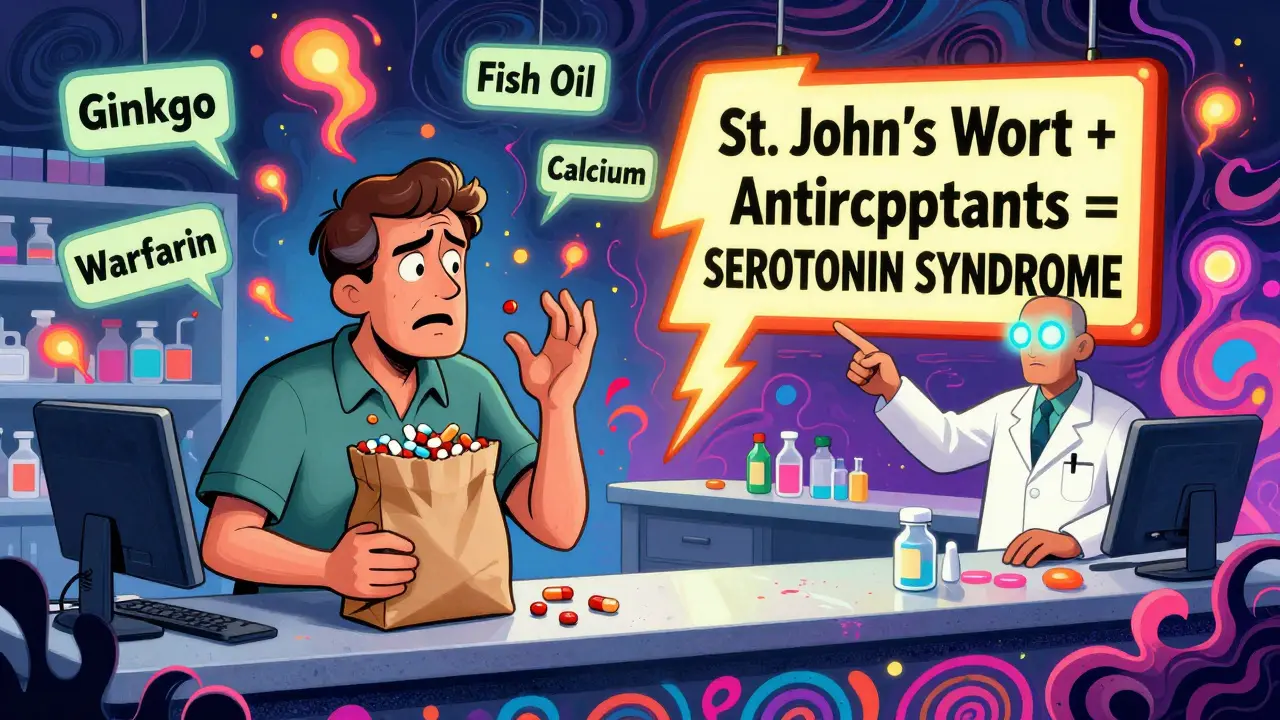
Supplements aren’t regulated like prescription medications. That means companies don’t have to prove they’re safe before selling them. The FDA only steps in after something goes wrong. And when it does, the results are often serious. St. John’s wort, for example, can cut the effectiveness of birth control pills by up to 50%. It can also make your transplant medication useless - meaning your body might reject the new organ. That’s not a side effect. That’s life-threatening. The problem isn’t just one or two bad actors. Over 57 prescription drugs interact dangerously with St. John’s wort, including antidepressants, HIV meds, and cholesterol-lowering drugs. Even something as common as vitamin E - at doses over 400 IU - can thin your blood so much that it causes internal bleeding if you’re on warfarin. And ginkgo biloba? It’s fine for most people. But if you’re taking Eliquis or Plavix, it can trigger a major bleed. One Reddit user reported a seven-day hospital stay after combining ginkgo with Eliquis. He didn’t tell his doctor he was taking it.Which Supplements Are Most Likely to Cause Problems?
Not all supplements are created equal. Some are low-risk. Others are ticking time bombs. Here’s the breakdown based on clinical evidence:- High-risk (avoid with most medications): St. John’s wort, goldenseal, kava, ephedra
- Moderate-risk (use with caution): Ginkgo biloba, garlic, ginger, fish oil, vitamin E (400 IU+)
- Low-risk (generally safe): Milk thistle, cranberry, American ginseng, saw palmetto, valerian
What About Minerals? Calcium, Iron, Zinc - Are They Safe?
Yes and no. Minerals like calcium, magnesium, zinc, and iron don’t interact with drugs the same way herbs do. But they compete with each other - and with your meds - for absorption. If you take iron and calcium together, your body absorbs less of both. That’s why some doctors tell you to take iron on an empty stomach and calcium with food. But here’s the real danger: if you’re on thyroid medication like levothyroxine, taking calcium or iron within four hours can block its absorption completely. That means your thyroid levels stay low, even if you’re taking your pill every day. The same goes for antibiotics like tetracycline or ciprofloxacin. These drugs bind to minerals and become useless. You might think you’re getting better - but you’re not.
How to Check for Interactions Before You Take Anything
You don’t need to be a pharmacist to protect yourself. Here’s what actually works:- Make a complete list - every pill, capsule, powder, and tea you take. Include dosages and how often you take them. Don’t forget vitamins, herbal teas, or CBD oil.
- Bring it to your doctor or pharmacist - every time. Not just once. Every new prescription, every new supplement. Ask: Does this interact with anything else I’m taking?
- Use the brown bag method - dump everything you take into a brown paper bag and bring it to your pharmacy. Pharmacists at CVS, Walgreens, and other chains are trained to spot interactions. In 2021, Walgreens started screening every customer who buys supplements. They found dangerous interactions in 18% of cases.
- Check the label - look for warning statements. If it says "Do not use if taking blood thinners" or "May interfere with antidepressants," pay attention. Most people skip this part.
- Use the FDA’s new tool - launching in late 2024, the Dietary Supplement Ingredient Database app lets you scan a supplement barcode and instantly see known interactions. It’s free. It’s official. And it’s coming soon.
When to Stop Taking a Supplement
There are times when you need to stop - immediately. If you’re scheduled for surgery, your doctor will likely tell you to stop taking garlic, ginkgo, fish oil, and vitamin E at least 7-10 days before. Why? Because they increase bleeding risk. One study found patients who kept taking fish oil before surgery had 3 times more blood loss. Also stop if you start feeling weird. Unexplained bruising, dizziness, nausea, rapid heartbeat, or confusion could be signs of a dangerous interaction. Don’t wait. Call your doctor. If you’re on warfarin and your INR suddenly spikes, it could be because you started taking a new supplement.What You Should Never Assume
Here are three dangerous myths:- Myth: "Natural means safe." Truth: Poison ivy is natural. Snake venom is natural. St. John’s wort is natural - and it can kill.
- Myth: "My doctor knows what I’m taking." Truth: A 2023 survey found 68% of supplement users never tell their doctor. Most doctors don’t ask - because they don’t know to.
- Myth: "I’ve been taking this for years without problems." Truth: Interactions can show up after months or years. Your body changes. Your meds change. What was fine last year might be dangerous now.
Who’s at the Highest Risk?
Adults over 50 are the most vulnerable group. Why? Because they’re more likely to take multiple prescriptions - and more likely to take supplements for joint pain, memory, or energy. According to the National Health Interview Survey, 78% of people over 50 take both. But only 32% talk to their doctor about their supplements. That’s a recipe for disaster. One wrong combo can send you to the hospital. And it’s not rare. The FDA logged over 3,200 supplement-related adverse events in 2022 - nearly half involved medication interactions.What’s Changing in 2025?
The system is slowly catching up. In June 2023, the American Medical Association made it mandatory for doctors to ask about supplements during every medication review. Epic Systems - the biggest electronic health record provider - now flags supplement-drug interactions in 15% of U.S. hospitals. And the FDA’s new labeling rules will require clearer warnings by 2026. But you can’t wait for the system to fix itself. The best protection is still you - being informed, asking questions, and speaking up.Final Checklist: Is Your Supplement Safe?
Before you take any new supplement, ask yourself:- Do I have a complete list of everything I take - meds, supplements, vitamins, teas?
- Have I shown this list to my doctor or pharmacist in the last 3 months?
- Does the supplement label have a warning about medications?
- Am I taking it with food, or on an empty stomach? (Some minerals need spacing.)
- Have I checked for interactions using a reliable source like the FDA’s upcoming app or MedlinePlus?
- Do I know what side effects to watch for - bruising, dizziness, nausea, heart palpitations?
Can I take St. John’s wort with my antidepressant?
No. St. John’s wort can cause serotonin syndrome when taken with SSRIs like Lexapro, Zoloft, or Prozac. This is a life-threatening condition that causes high fever, rapid heartbeat, confusion, seizures, and muscle rigidity. Even if you feel fine at first, the risk builds over time. The FDA and NCCIH both warn against this combination.
Is it safe to take fish oil with blood thinners?
It depends. Fish oil has mild blood-thinning effects. If you’re on warfarin, Eliquis, or Plavix, taking high doses (over 3,000 mg daily) can increase your risk of bleeding. Some doctors allow low doses (1,000 mg) with close monitoring. But most recommend avoiding it entirely if you’re on strong anticoagulants. Always check with your pharmacist before combining them.
Do I need to stop supplements before surgery?
Yes - and you should do it at least 7 to 10 days before. Supplements like garlic, ginkgo, ginger, fish oil, and vitamin E can interfere with blood clotting during and after surgery. Even if your surgeon doesn’t mention it, bring your supplement list to your pre-op appointment. Many hospitals now require this.
Can calcium interfere with my thyroid medication?
Yes. Calcium supplements - including antacids with calcium - can block your body from absorbing levothyroxine. Take them at least 4 hours apart. Same goes for iron, magnesium, and even soy milk. If your thyroid levels aren’t improving, this could be why.
Are there any supplements that are safe with almost all medications?
Yes - milk thistle, cranberry, American ginseng, and valerian have very few documented interactions. But "few" doesn’t mean "none." Always check. Even safe supplements can react differently based on your health, liver function, or other drugs. There’s no universal "safe" supplement - only ones with lower risk.
What should I do if I think a supplement is making me sick?
Stop taking it immediately. Write down what you took, when, and what symptoms you’re having. Call your doctor or go to urgent care. Then report it to the FDA through their MedWatch system. Your report helps protect others. Don’t assume it’s just a coincidence - supplement interactions are underreported and often missed.
If you’re taking medications - especially for heart disease, depression, diabetes, or transplant recovery - don’t guess about supplements. Talk to your pharmacist. Bring your brown bag. Ask the question. Your life might depend on it.
Aditya Kumar
Been taking turmeric for my knees for years. Never thought to check if it played nice with my blood pressure med. Guess I’m lucky so far. Still, I’ll bring my brown bag to the pharmacy next time. Better safe than sorry.
Also, why does no one ever talk about how supplements cost 10x more than they should? Like, it’s just ground-up plants in a capsule. The markup is insane.
Colleen Bigelow
THIS is why America is falling apart. Big Pharma doesn’t want you to know the truth - supplements are safer than their poison pills, but they’ve bought off the FDA to scare you into staying dependent. St. John’s wort? It’s been used for centuries. The real danger is corporate greed hiding behind ‘clinical evidence.’
They’re lying to you. Always have been. Wake up.
Also, the FDA’s new app? Probably a backdoor to track your supplement use. I’m not falling for it. Bring your brown bag? Nah. I’ll bring my own damn bag - and my own damn truth.
Billy Poling
It is of paramount importance to underscore that the regulatory framework governing dietary supplements in the United States is fundamentally distinct from that of pharmaceutical agents, which are subject to rigorous pre-market approval protocols under the Federal Food, Drug, and Cosmetic Act. Consequently, the absence of mandatory pre-market safety and efficacy data for botanical products creates a significant information asymmetry between consumers and manufacturers, thereby elevating the probability of adverse pharmacodynamic interactions, particularly among polypharmacy populations. For instance, the cytochrome P450 enzyme induction mediated by hypericum perforatum (St. John’s wort) demonstrably reduces serum concentrations of cyclosporine, tacrolimus, and oral contraceptives, thereby compromising therapeutic efficacy and precipitating clinically significant outcomes such as organ rejection or unintended pregnancy. Moreover, the pharmacokinetic interference between mineral supplements and levothyroxine absorption, mediated by chelation in the gastrointestinal lumen, necessitates temporal separation of administration by a minimum of four hours, a behavioral modification frequently overlooked by patients and clinicians alike. The utility of the brown-bag method, as endorsed by the American Pharmacists Association, remains an underutilized yet highly effective risk mitigation strategy, particularly in community pharmacy settings where pharmacists serve as the most accessible point of clinical intervention. Therefore, it is imperative that all patients undergoing polypharmacy regimens engage in proactive, structured disclosure of all ingested substances - including botanicals, vitamins, and over-the-counter preparations - during every clinical encounter, irrespective of perceived relevance or duration of use.
Kim Hines
My grandma took ginkgo for her memory and warfarin for her atrial fibrillation. She ended up in the ER with a brain bleed. They didn’t know she was taking it. She never told anyone. I still think about it.
Just… be careful.
Joanna Ebizie
Oh wow, so you’re telling me that the ‘natural’ stuff I’ve been buying at Whole Foods is basically a gamble with my liver? And I thought I was being healthy.
Y’all are lucky you’re not dead yet. I stopped taking everything except my multivitamin after I read about someone’s kidneys shutting down from ‘herbal detox tea.’
Also, vitamin E? 400 IU? That’s not a supplement, that’s a dare.
Mike Smith
This is one of the most important posts I’ve read in years. Thank you for laying it out so clearly. I’m a nurse, and I see this every single week - people come in with bleeding, confusion, or organ rejection, and they swear they didn’t take anything ‘medicinal.’
Don’t be ashamed to ask. Don’t assume your doctor knows. Don’t trust labels that say ‘natural.’
Bring your brown bag. Write it down. Ask your pharmacist. You’re not being paranoid - you’re being smart.
And if you’re over 50? Please, please, please - this isn’t optional. Your life depends on it.
Ron Williams
I’m from the Philippines and we use a lot of herbal remedies here - turmeric, ginger, sambong. My cousin’s dad took sambong with his blood pressure meds and ended up with low potassium. No one told him it could interact.
It’s not just an American problem. This is global. We need better education in every language.
Also, I’m glad the FDA’s app is coming. I’ll be the first to download it and translate it into Tagalog for my family.
Kitty Price
Just started taking fish oil for my joints. I’m gonna check with my pharmacist tomorrow before I take another pill. 🙏
Also - I’m printing out that checklist and taping it to my medicine cabinet. Because I’m the type to forget everything until I’m in the ER.
Randolph Rickman
Look - I used to think supplements were just ‘bonus health.’ Now I know they’re like adding another driver to your car without telling the mechanic.
It’s not about being afraid. It’s about being responsible.
Take 30 seconds. Make a list. Ask your pharmacist. It’s that simple.
You don’t need to be a scientist. You just need to care enough to ask.
And if you’re reading this and thinking ‘I’m fine’ - you’re not. Not until you’ve checked.
sue spark
I took St John's wort for a year thinking it was just a mild mood booster. Then I got pregnant and found out it probably didn't work because my birth control was useless. I didn't even know. I'm so mad at myself. Don't be like me.
SHAMSHEER SHAIKH
As a clinical pharmacist with over 22 years of experience, I have personally witnessed over 89 cases of life-threatening interactions involving herbal supplements - and in 92% of those cases, the patient had never disclosed the supplement use to any healthcare provider. The most alarming trend? Patients believe that because a product is labeled as ‘pure’ or ‘traditional,’ it is inherently safe - a dangerous fallacy. The liver metabolizes every substance - whether it’s a synthetic drug or a botanical extract - and when two or more agents compete for the same enzyme pathways, the outcome is not a matter of chance, but of biochemistry. I urge every patient: maintain a written log, update it monthly, and present it to your prescriber during every visit - even if you think it’s ‘just a tea.’ Your life is not a gamble - it is a responsibility.
And yes - the FDA’s new app is a step forward. But knowledge must precede technology. Educate yourself first.
James Rayner
I’ve been thinking about this a lot lately - how we treat our bodies like machines you can upgrade with random parts from the internet.
We’ll install a new app on our phone and read 10 reviews before we hit download. But we’ll swallow a capsule with no idea what’s inside, who made it, or what it’s doing to our liver.
Maybe the problem isn’t the supplements.
Maybe it’s that we’ve forgotten how to be careful.
Not scared. Just careful.
And maybe we need to start again.
Souhardya Paul
My dad took calcium with his thyroid med for years and his TSH was always off. We didn’t figure it out until his endocrinologist asked him about his morning routine - turns out he took his calcium with breakfast, right after his pill.
He’s been fine since he started taking calcium at night.
So yeah - timing matters. And asking questions isn’t annoying. It’s essential.
Also - I printed this whole post and gave it to my mom. She’s 72. She’s on 7 meds. She didn’t even know she should tell her doctor about her fish oil.
Josias Ariel Mahlangu
Supplements are a scam. The government lets them sell poison because they’re too lazy to regulate it. And you people just keep buying it. You’re not being smart. You’re being manipulated.
Stop wasting your money. Stop trusting ‘natural’ labels. The only safe supplement is the one your doctor prescribes - and even then, you should still ask questions.
Stop being gullible.