Leukemia-Anemia Connection Quiz
About This Quiz
This interactive quiz helps you understand key concepts about how leukemia and anemia are connected. Test your knowledge and learn more about the causes, symptoms, and management strategies.
Quiz Results
Quick Takeaways
- Leukemia often leads to anemia because cancerous cells crowd out healthy blood‑forming cells in the bone marrow.
- Both acute and chronic forms can cause low red‑cell counts, but the speed and severity differ.
- Common symptoms overlap: fatigue, shortness of breath, and pale skin.
- Blood tests, bone‑marrow biopsy, and iron studies are essential for proper diagnosis.
- Treatment‑related anemia can be managed with transfusions, iron supplementation, and growth‑factor drugs.
Understanding how leukemia and anemia interact helps patients and caregivers spot warning signs early and work with doctors on a treatment plan that tackles both issues.
What Is Leukemia?
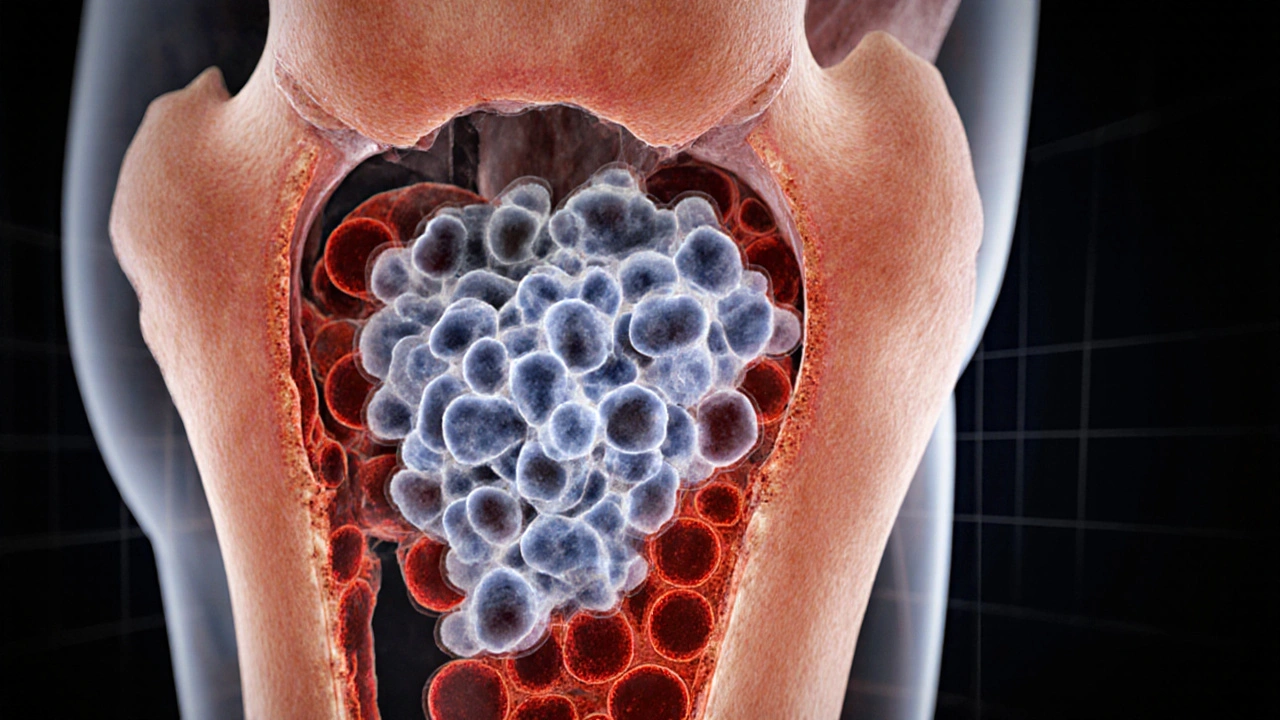
Leukemia is a cancer of the blood‑forming tissues, most commonly the bone marrow, that results in the uncontrolled production of abnormal white blood cells. These malformed cells crowd out normal blood components, impairing the body’s ability to fight infection, clot blood, and carry oxygen.
What Is Anemia?
Anemia is a condition marked by a deficiency in red blood cells (RBCs) or hemoglobin, reducing the blood’s oxygen‑transport capacity. Symptoms range from mild fatigue to severe shortness of breath and heart strain.
Why Does Leukemia Lead to Anemia?
The connection boils down to three physiological mechanisms:
- Bone‑marrow crowding: Cancerous white blood cells (WBCs) proliferate inside the bone marrow, physically displacing the progenitor cells that generate red blood cells, platelets, and healthy white cells.
- Disrupted differentiation: Leukemic blasts often block the normal maturation pathway of red blood cells, causing many immature cells to die before they can enter circulation.
- Treatment side effects: Chemotherapy and targeted therapies, while killing cancer cells, also damage rapidly dividing marrow cells, leading to a temporary drop in RBC production.

Types of Leukemia and Their Anemia Profiles
Not all leukemias affect blood counts the same way. Below is a snapshot of the most common subtypes and how they typically influence anemia.
| Leukemia Type | Onset | Average Hemoglobin Drop (g/dL) | Common Anemia Cause |
|---|---|---|---|
| Acute Lymphoblastic Leukemia (ALL) | Weeks | 3‑5 | Bone‑marrow infiltration |
| Acute Myeloid Leukemia (AML) | Weeks | 4‑6 | Marrow failure + chemotherapy |
| Chronic Lymphocytic Leukemia (CLL) | Months‑years | 1‑2 | Autoimmune hemolysis |
| Chronic Myeloid Leukemia (CML) | Months‑years | 1‑3 | Therapy‑induced marrow suppression |
Shared Symptoms: When to Suspect Both Conditions
Because anemia reduces oxygen delivery, many of its signs mimic those of leukemia itself. Keep an eye out for these overlapping clues:
- Persistent fatigue that doesn’t improve with rest.
- Pale or yellowish skin, especially on the inner eyelids.
- Shortness of breath during mild activity.
- Rapid heart rate (palpitations) at rest.
- Unexplained bruising or frequent infections (points more to leukemia but often appear together).
If you notice a combination of these signs, especially alongside night sweats or unexplained weight loss, seek a medical evaluation promptly.
How Doctors Diagnose the Overlap
Diagnosis hinges on a series of blood and marrow tests:
- Complete Blood Count (CBC): Reveals low hemoglobin, hematocrit, and abnormal white‑cell counts.
- Peripheral Blood Smear: Shows the shape of RBCs and the presence of blast cells.
- Bone‑Marrow Biopsy: Samples bone marrow to identify leukemic infiltration and assess cellularity.
- Iron Studies: Serum ferritin, transferrin saturation, and total iron‑binding capacity help differentiate iron‑deficiency anemia from anemia of chronic disease.
- Cytogenetic & Molecular Tests: Detect genetic mutations (e.g., BCR‑ABL, FLT3) that guide targeted therapy.
These results together paint a clear picture of how the two diseases intersect.
Treatment‑Related Anemia: What to Expect
Even after leukemia is under control, anemia can linger. Common culprits include:
- Chemotherapy: Damages rapidly dividing marrow cells, causing a nadir (lowest point) around 7‑14 days post‑treatment.
- Targeted therapy (e.g., tyrosine‑kinase inhibitors): May cause mild to moderate anemia as a side effect.
- Immune‑mediated hemolysis: Some drugs trigger the body to destroy its own red cells.
Doctors monitor blood counts before each chemotherapy cycle and intervene when hemoglobin falls below 8g/dL (or higher for patients with heart disease).
Managing Anemia in Leukemia Patients
Effective management blends medical interventions with lifestyle tweaks:
- Blood Transfusions: Quick way to restore oxygen‑carrying capacity, especially during intense treatment phases.
- Erythropoiesis‑Stimulating Agents (ESAs): Drugs like darbepoetin can stimulate red‑cell production, but they’re used cautiously because of thrombosis risk.
- Iron Supplementation: Oral or IV iron is prescribed if iron‑deficiency coexists. Iron deficiency is less common in leukemia‑related anemia but can appear after chronic blood loss.
- Nutrient‑Rich Diet: Foods high in vitamin B12, folate, and iron (lean meat, leafy greens, legumes) support marrow recovery.
- Exercise: Light aerobic activity boosts circulation and can improve fatigue, but it should be cleared by an oncologist.
Regular follow‑up labs help fine‑tune these strategies.
When Anemia Signals a Relapse
A sudden, unexplained drop in hemoglobin, especially if accompanied by a rise in blast cells, may hint that leukemia is returning. In such cases, doctors typically repeat the bone‑marrow biopsy and adjust therapy accordingly.
Key Takeaway Checklist
- Leukemia interferes with red‑cell production via marrow crowding, blocked differentiation, and treatment toxicity.
- Acute leukemias cause rapid, severe anemia; chronic forms often lead to milder, long‑term anemia.
- Overlap of fatigue, pallor, and shortness of breath warrants prompt blood work.
- Management includes transfusions, ESAs, iron therapy, and supportive nutrition.
- Monitor hemoglobin trends; sharp declines can signal relapse.
Frequently Asked Questions
Can leukemia cause iron‑deficiency anemia?
Iron‑deficiency anemia is usually the result of chronic blood loss or poor dietary intake. In leukemia, anemia more often stems from marrow suppression rather than iron shortage. However, if a patient experiences gastrointestinal bleeding from chemotherapy‑induced ulcers, iron loss can occur, so doctors may check iron studies alongside the CBC.
Is a blood transfusion safe for someone undergoing chemotherapy?
Yes, transfusions are a standard supportive measure. They are filtered and matched to reduce the risk of reactions. The main concerns are iron overload from repeated transfusions and potential immunologic effects, which clinicians monitor closely.
How long does it take for anemia to improve after chemotherapy ends?
Recovery varies. For most patients, red‑cell counts start rising 2‑4 weeks after the last chemo cycle, reaching baseline within 2‑3 months. Factors like age, baseline marrow reserve, and whether ESAs were used influence the timeline.
Do all leukemias require the same anemia management?
No. Acute leukemias often need aggressive transfusion support during induction therapy, while chronic leukemias may be managed with occasional iron supplementation and monitoring, unless treatment side effects cause a drop.
Can lifestyle changes reduce anemia risk in leukemia patients?
A balanced diet rich in B‑vitamins, folate, and iron helps the marrow recover quicker. Light exercise, approved by the oncologist, can boost circulation and reduce fatigue. However, these measures complement-not replace-medical treatment.
Sahithi Bhasyam
Wow, the way leukemia crowds out the marrow is like a bustling market where the stalls overtake the walkways,, making it hard for anyone to get through! The article captures that bone‑marrow crowding nicely, even though I wish they'd've added a bit more on cultural dietary impacts-some foods can actually help the marrow bounce back,, you know? Also, the connection between fatigue and low oxygen is spot on; it's something we see in many Indian patients who also face nutritional challenges. Great job breaking down complex science into readable chunks 😊
mike putty
Reading through the explanations about anemia management really lifts my spirits, especially the part about blood transfusions being a quick fix during intensive chemo. It’s comforting to know that doctors monitor hemoglobin closely and step in before patients feel too weak. The lifestyle tips like gentle exercise and iron‑rich foods are practical and hopeful. Keep sharing these helpful insights!
Kayla Reeves
Frankly, the article glosses over the ethical dilemmas of frequent transfusions.
Abhinanda Mallick
One must acknowledge the gravitas of marrow invasion, a battlefield where malignant progeny annihilate the noble lineage of erythrocytes. The discourse, though thorough, could have benefitted from a more incisive critique of therapeutic complacency that pervades our institutions. It is incumbent upon the medical elite to champion aggressive interventions, lest we resign to a passive acceptance of anemia’s tyranny. Moreover, the omission of socio‑economic disparities in treatment access betrays a myopic perspective. Let us demand a paradigm shift that elevates both scientific rigor and national resolve.
Richard Wieland
Leukemia‑induced anemia exemplifies how a disruption in one cellular lineage cascades into systemic fatigue, underscoring the interconnectedness of hematopoiesis. Understanding this cascade aids clinicians in anticipating transfusion needs and tailoring supportive care.
rachel mamuad
Building on the supportive tone, the concept of erythropoietic‑stimulating agents (ESAs) acts as a pharmacologic lever to augment RBC production amidst marrow aplasia. While the term "growth‑factor modulation" may sound esoteric, its clinical relevance lies in reducing transfusion dependency-an outcome that resonates across the hematology‑oncology spectrum. Of course, cost‑effectivness analyses (CEAs) must be integrated into decision‑making frameworks to ensure equitable resource allocation, especially in low‑income settings.
Amanda Anderson
It hits hard when you realize those cancerous cells are like invaders storming the factory, shutting down the workers that make our blood. The fatigue that follows is more than just tiredness-it's a signal that the body is crying out for help. Seeing this laid out so plainly helps patients grasp why they feel so weak.
Carys Jones
While many hail the article as comprehensive, it fails to confront the harsh reality that some treatment protocols prioritize remission statistics over patient quality of life. The relentless pursuit of blast eradication often sidelines the individual's struggle with chronic anemia, leading to a cascade of secondary complications. This oversight reflects a systemic flaw where numbers eclipse humane care.
Roxanne Porter
Indeed, balancing remission metrics with supportive care is essential. Integrating routine anemia assessments into treatment algorithms can mitigate the risk of overlooking patient well‑being. Collaborative multidisciplinary meetings foster a holistic approach that aligns therapeutic goals with quality‑of‑life considerations.
Jonathan Mbulakey
Reflecting on the balance between aggressive treatment and supportive care highlights the ethical nuances inherent in oncology. Patient preferences should steer decisions whenever feasible.
Warren Neufeld
The overview of iron studies versus CBC really clarifies how clinicians differentiate anemia types, which can be confusing for patients. Simple explanations like these empower families to ask informed questions during appointments.
Deborah Escobedo
Absolutely, using clear language when discussing iron studies helps patients understand whether supplementation or transfusion is appropriate. Providing pamphlets with visual aids can further enhance comprehension without overwhelming the reader.
Dipankar Kumar Mitra
Yo, that skinny explanation about marrow crowding misses the drama of the cellular war zone. Blood cells are like soldiers being trampled by a relentless horde of leukemic bots, and you can't just brush it off with a bland sentence. We need to feel the urgency, the desperation of the body screaming for oxygen. Don't let the science get too sterile; inject some humanity into the narrative!
Tracy Daniels
Understanding the intricate dance between leukemia and anemia is a cornerstone of compassionate patient care. When malignant blasts invade the marrow, they displace the progenitor cells that would normally mature into healthy red blood cells. This displacement reduces the oxygen‑carrying capacity of the blood, leading to the classic symptom of fatigue that many patients describe as an overwhelming lassitude. Additionally, chemotherapy agents, while targeting the cancerous cells, also temporarily suppress the bone‑marrow's regenerative ability. Therefore, clinicians often anticipate a nadir in hemoglobin levels roughly one to two weeks after a treatment cycle. Proactive monitoring through regular complete blood counts allows for timely interventions before the patient becomes symptomatic. One of the most effective supportive measures is the judicious use of packed red blood cell transfusions, which can swiftly restore oxygen delivery. However, repeated transfusions carry risks such as iron overload, necessitating careful assessment of cumulative exposure. Erythropoiesis‑stimulating agents may be considered in select cases, but their use must be balanced against potential thrombotic complications. Nutritional support, including adequate intake of iron, vitamin B12, and folate, synergizes with medical therapies to promote marrow recovery. Encouraging light, physician‑approved physical activity can also improve circulation and reduce fatigue, fostering a sense of agency in patients. It is equally important to address the psychological impact of concurrent leukemia and anemia, as chronic tiredness can exacerbate anxiety and depression. Integrating psychosocial resources, such as counseling and support groups, creates a holistic treatment environment. Finally, clear communication-using plain language, visual aids, and empathetic listening-empowers patients to participate actively in their care decisions. By weaving together these medical and supportive strategies, we can mitigate the burden of anemia while fighting leukemia, ultimately enhancing quality of life 😊.