When you’re pregnant and managing a mental health condition, the question isn’t just whether to take medication-it’s how to make the best choice for you and your baby. Too often, people are left to guess, scared by old warnings or half-truths. But the truth is simpler: there’s no risk-free option. Stopping medication can be just as dangerous as taking it. That’s why shared decision-making isn’t just a buzzword-it’s the standard of care.
Why This Isn’t Just About Medication
Untreated depression, anxiety, or bipolar disorder during pregnancy doesn’t just affect how you feel. It affects your baby too. Studies show that when mental illness goes unmanaged, the risk of preterm birth goes up by 62%. The chance of having a baby with low birth weight increases. And yes-there’s a 20% higher risk of maternal suicide. These aren’t rare outcomes. They’re real, measurable, and preventable. On the other side, people worry about birth defects. The fear of a heart problem or a neural tube defect can feel overwhelming. But here’s the thing: the risk from medication is often smaller than the risk from not treating the illness. For example, paroxetine (Paxil) increases the chance of a heart defect from about 8 in 1,000 births to 10 in 1,000. That’s a 2-per-thousand increase. Meanwhile, untreated depression raises preterm birth risk by 30% to 50%. That’s not a small trade-off.What Medications Are Actually Safe?
Not all psychiatric medications are the same. Some have strong safety data. Others should be avoided. Here’s what the latest guidelines say:- SSRIs like sertraline (Zoloft), citalopram (Celexa), escitalopram (Lexapro), and fluoxetine (Prozac) are first-line choices. They’re the most studied, and most show no major increase in birth defects-except paroxetine. If you’re on paroxetine, switching before pregnancy is often recommended.
- Lamotrigine is the go-to for bipolar disorder. It doesn’t cause major birth defects, unlike valproic acid, which can raise the risk of neural tube defects from 0.1% to 1-2%. That’s a 10- to 20-fold increase. Valproic acid is off the table for anyone who could get pregnant.
- Bupropion (Wellbutrin) has a small link to miscarriage and heart issues. It’s not first-choice, but it’s an option if SSRIs don’t work.
- Tricyclics like nortriptyline and amitriptyline are older but still used when newer meds fail. They’re not perfect, but they’re better than leaving depression untreated.
- Typical antipsychotics like haloperidol and chlorpromazine have decades of safe use. Atypical ones? Not so much. We just don’t have enough long-term data on kids exposed to risperidone or quetiapine in the womb.
The American College of Obstetricians and Gynecologists (ACOG) and the British Association for Psychopharmacology both agree: if you need medication to stay stable, it’s usually safer to stay on it.
Shared Decision-Making: What It Actually Looks Like
This isn’t a one-time chat. It’s a process. And it starts before you even get pregnant.Here’s how it works:
- Assess your risk. Have you had depression before? How many episodes? How severe? If you’ve had a hospitalization or a suicide attempt, your risk of relapse during pregnancy is over 80% if you stop meds. That’s not speculation-it’s data.
- Know the numbers. Don’t just hear “it’s risky.” Ask: “What’s the actual chance?” For example: “Paroxetine raises the risk of a heart defect from 8 in 1,000 to 10 in 1,000.” That’s 2 extra cases per 1,000 births. Compare that to the 30-50% higher risk of preterm birth if you stop your antidepressant.
- Plan for setbacks. What if your anxiety spikes at 20 weeks? What if you can’t sleep? Have a clear plan: when to call your provider, when to adjust dose, when to add therapy. No one should be left guessing.
Tools like the Mental Health Medication Decision Aid from ACOG give providers real-time data on 24 medications, updated every quarter. You should get a copy. Read it. Ask questions. Bring it to your next appointment.
What the Data Says About Discontinuing
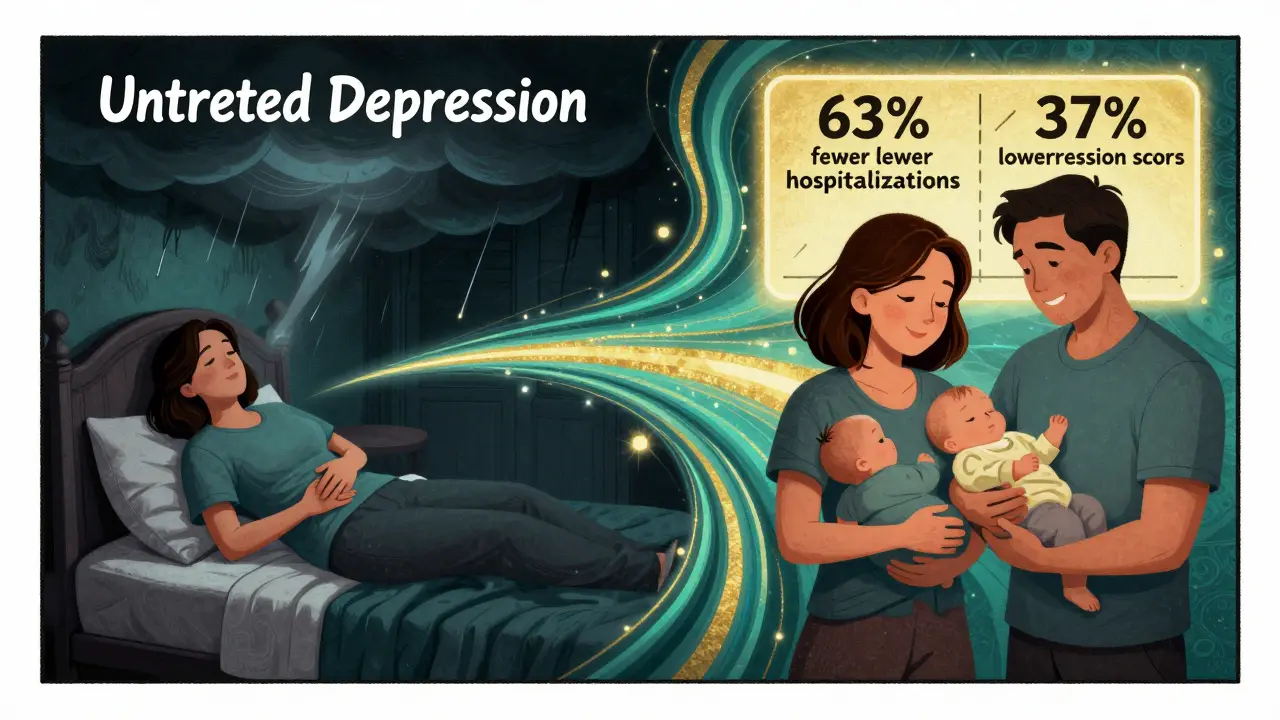
A lot of people stop their meds because they’re scared. But the consequences are often worse.The National Pregnancy Registry for Psychiatric Medications tracked over 15,000 women since 2010. They found that 68% didn’t get clear info before getting pregnant. And 42% stopped meds on their own-no doctor involved. Of those, 63% reported worse symptoms, hospitalization, or even suicidal thoughts after stopping.
Reddit threads from r/PostpartumDepression show the same pattern. Out of 1,243 posts, 78% said they were pressured to quit meds. Many did-and ended up in crisis. One woman wrote: “I stopped sertraline because my OB said ‘it’s better for the baby.’ I had a panic attack so bad I called 911 at 18 weeks.”
On the flip side, women who used shared decision-making tools were 3.2 times more likely to stick with their treatment. And six weeks after birth, they had 37% lower depression scores.
What’s New in 2026?
The science is moving fast. In 2023, ACOG updated its guidelines to say: when you control for the underlying mental illness, most studies show no clear link between medication and long-term harm to children. That’s huge. It means the real danger isn’t the pill-it’s the untreated illness.The National Pregnancy Registry is now tracking 12 new medications, including brexpiprazole, which has almost no data. And by 2026, tools will start using machine learning to give you personalized risk estimates-not just population averages. If you’re a 32-year-old with two prior depressive episodes, your risk of relapse might be 85%. If you’re 26 with mild anxiety and no history, it might be 40%. That’s the future.
Right now, 87% of obstetricians consult perinatal psychiatrists before prescribing. That’s up from 42% in 2015. The system is catching up. But you still have to push for it.

What You Can Do Right Now
If you’re planning a pregnancy or already pregnant:- Don’t stop medication without talking to your provider. Not even for one day.
- Ask for the Mental Health Medication Decision Aid. If they don’t have it, ask why.
- Track your mood. Use a simple app or journal. Note sleep, energy, panic attacks. This helps your provider adjust your plan.
- Bring someone with you to appointments. A partner, friend, or doula. You’re not expected to remember everything.
- If your provider dismisses your concerns, find someone who listens. Perinatal psychiatrists exist for this reason.
There’s no perfect choice. But there is a better one: an informed one. You deserve to make that choice without fear, shame, or pressure.
Are SSRIs safe during pregnancy?
Yes, most SSRIs are considered safe. Sertraline, citalopram, escitalopram, and fluoxetine have strong safety data and are recommended as first-line treatments. Paroxetine is the exception-it’s linked to a small increase in heart defects and should be avoided if possible. Switching to another SSRI before or during pregnancy is often advised.
Can I breastfeed while taking mental health meds?
Most antidepressants and mood stabilizers are safe during breastfeeding. Sertraline is often the top choice because it passes into breast milk in very low amounts. Fluoxetine can build up over time, so it’s less preferred. Lithium requires careful monitoring, but it’s still used with proper dosing. Always check with your provider-each medication has its own profile.
What if I’m on lithium or valproic acid and just found out I’m pregnant?
Call your provider immediately. Valproic acid should be stopped as soon as possible-it’s linked to neural tube defects and developmental delays. Lithium needs careful management because your body processes it differently during pregnancy. Your team will likely switch you to lamotrigine, which is much safer. Don’t panic-this is manageable with the right support.
Is therapy enough instead of medication?
For mild depression or anxiety, therapy alone can work. But if you’ve had moderate to severe episodes, especially with hospitalizations or suicidal thoughts, therapy alone is often not enough. Medication helps stabilize your brain chemistry so therapy can be more effective. They’re not alternatives-they’re partners.
How do I know if my provider is doing shared decision-making right?
They should give you clear numbers-not vague warnings. They should ask what matters to you. Do you value sleep over avoiding all risk? Do you fear hospitalization more than birth defects? They should offer options, explain trade-offs, and document your choice. If they say “just stop” or “it’s fine,” that’s not shared decision-making. That’s directive-and it’s outdated.
Can I get help even if I’m not in a big city?
Yes. Many hospitals now offer telehealth perinatal psychiatry services. National Pregnancy Registry partners and organizations like Postpartum Support International connect people with specialists across Australia and beyond. You don’t need to be near a university hospital to get expert care.
