What Are Silicosis and Asbestosis?
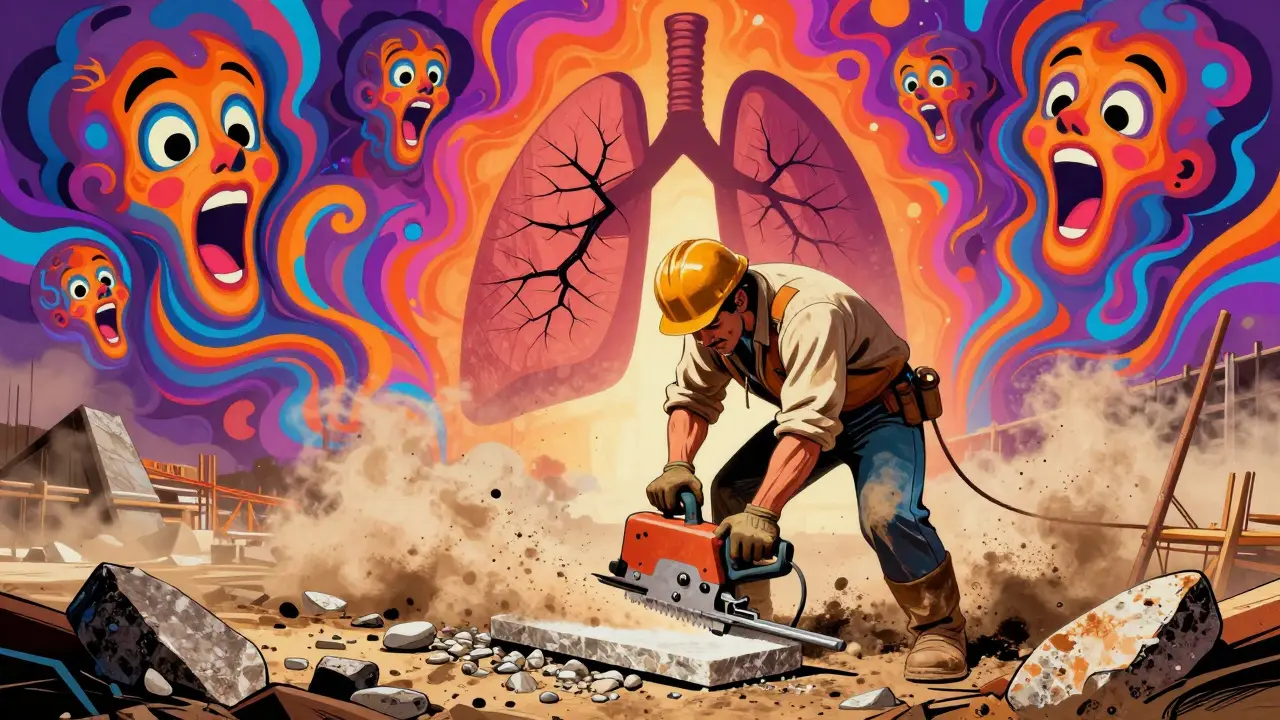
Silicosis is a lung disease caused by breathing in tiny particles of crystalline silica, a mineral found in sand, stone, and concrete. When workers cut, grind, or drill materials like granite, quartz, or engineered stone, they release dust that gets deep into the lungs. Over time, this dust triggers scarring - stiff, fibrous tissue replaces healthy lung tissue. The result? Reduced lung capacity, chronic cough, and trouble breathing. It doesn’t show up overnight. Most cases develop after 10-30 years of exposure, but aggressive forms can appear in just 5-10 years if dust levels are high.
Asbestosis is a similar but distinct condition caused by inhaling asbestos fibers, once widely used in insulation, roofing, and fireproofing. These fibers are sharp and durable, lodging in lung tissue and causing inflammation that turns into permanent scarring. Like silicosis, it progresses slowly. Symptoms - shortness of breath, chest tightness, dry cough - often appear decades after exposure. The worst part? Once the damage is done, it can’t be reversed.
Both diseases are irreversible and can lead to serious complications: lung cancer, heart failure, and respiratory failure. And here’s the hard truth: neither disease has a cure. Treatment focuses on slowing progression, managing symptoms, and improving quality of life. That’s why prevention isn’t just important - it’s the only real solution.
Why These Diseases Are Still Happening in 2026
You’d think we’d have this figured out by now. After all, silicosis was first documented in Roman stonecutters over 2,000 years ago. Asbestosis was identified in a London factory worker in 1906. We’ve had the science for over a century. So why are people still getting sick?
Because prevention isn’t about knowledge - it’s about enforcement. In construction, demolition, and manufacturing, shortcuts still happen. A worker might skip a wet saw because it slows them down. A foreman might ignore respirator fit tests because they’re "a hassle." A small business might not have the budget for ventilation systems. And in many places, inspections are rare.
OSHA cited over 1,000 construction companies for silica violations in 2021. In the U.S. alone, between 2004 and 2014, over 1,100 workers died from asbestosis. NIOSH estimates 1,200 deaths each year from silicosis. These aren’t accidents. They’re preventable tragedies.
And it’s not just older workers. Younger people are getting hit too. Engineered stone countertops - popular in kitchens and bathrooms - contain up to 90% silica. Workers cutting these slabs without proper controls are developing aggressive silicosis in their 20s and 30s. This isn’t just a mining problem anymore. It’s a kitchen renovation problem.
The Hierarchy of Controls: What Actually Works
Not all protection is created equal. The CDC and NIOSH have a clear ranking of how to stop exposure - called the Hierarchy of Controls. It goes from most effective to least:
- Elimination - Don’t use silica or asbestos at all. Replace engineered stone with low-silica alternatives like quartz composites with less than 1% crystalline silica.
- Substitution - Use materials with lower hazard potential. For example, switch from dry-cutting stone to wet-cutting methods.
- Engineering Controls - These are the most reliable. Local exhaust ventilation systems that pull dust away at 100-150 feet per minute can reduce exposure by 80-90%. Wet cutting cuts silica dust by 90%. Enclosing the work area captures 95% of particles.
- Administrative Controls - Limit exposure time. Rotate workers. Schedule dusty tasks for low-traffic hours. Training helps, but alone, it only cuts exposure by 50-70%.
- PPE (Personal Protective Equipment) - Respirators are the last line of defense. N-95 masks filter 95% of particles. P-100 masks filter 99.97%. But here’s the catch: if the mask doesn’t fit, it’s useless. OSHA requires annual fit testing. Yet, CDC data shows 68% of complaints about respirators are about discomfort or poor fit. Workers often remove them, modify them, or don’t wear them at all - especially in 90°F heat.
Here’s the bottom line: engineering controls work. PPE only works if it’s used correctly - and too often, it isn’t.

What Workers and Employers Can Do Right Now
If you’re a worker: don’t wait for OSHA to show up. Ask for wet cutting tools. Demand a fit test for your respirator. Report unsafe conditions. You have legal rights under OSHA’s Whistleblower Protection Program. No one can fire you for speaking up.
If you’re an employer: start with the basics.
- Install local exhaust ventilation on every saw, grinder, or drill that creates dust.
- Use water spray systems for cutting, drilling, or polishing stone.
- Provide P-100 respirators - not just N-95s - and test them annually.
- Store respirators in clean, sealed containers. Don’t let them sit on the floor or in a toolbox with dirt and grease.
- Train workers for 4-6 hours initially, not the minimum 2. Include real-life scenarios. Show them what silicosis looks like on an X-ray.
- Get spirometry tests done. Baseline test when they start. Repeat every 5 years. Annually if they already have breathing issues.
Small businesses worry about cost. But here’s the math: a local exhaust system costs $2,000-$5,000 per workstation. That’s a one-time investment. The average workers’ compensation claim for silicosis or asbestosis? Over $250,000. The return on investment? Usually paid off in 18-24 months.
Why Smoking Makes Everything Worse
Smoking doesn’t cause silicosis or asbestosis. But it makes them far more dangerous.
The American Lung Association says smokers exposed to silica or asbestos have a 50-70% higher risk of developing lung disease. Smoking damages the lungs’ natural cleaning system - the cilia that sweep out dust and toxins. Add asbestos fibers or silica particles to that broken system, and the damage multiplies.
It also increases the risk of lung cancer. Asbestos and smoking together? That combination raises lung cancer risk by 50 times compared to non-smokers with no exposure. Quitting smoking isn’t just about health - it’s a critical part of workplace safety.

What’s Changing in 2026
There’s progress. NIOSH launched the "Prevent eTool" in 2023 - a free digital guide for 15 high-risk industries. Companies using it saw a 40% drop in respiratory incidents in six months.
OSHA’s National Emphasis Program on silica has conducted over 1,200 inspections since late 2022. Fines are climbing. The European Union is tightening asbestos limits by 2025. Germany’s pilot programs are cutting new cases by 55% with mandatory health monitoring.
But the biggest shift? It’s cultural. Companies that treat safety like a checklist fail. Those that treat it like a core value - where supervisors wear PPE every day, where workers speak up without fear, where health is measured as much as productivity - those are the ones succeeding.
Wearable sensors that track real-time dust exposure are starting to appear on job sites. They’re not perfect yet, but they’re a step toward accountability. The future of prevention isn’t just better masks - it’s better systems, better data, and better respect for the people doing the work.
Final Reality Check
These diseases are not inevitable. They are not "part of the job." They are the result of choices - choices about safety, about money, about priorities.
Every worker who breathes in silica or asbestos dust is taking a silent bet: that they won’t be the one who gets sick. But the odds are stacked against them. And when they do get sick, there’s no recovery. Only management.
Prevention works. We’ve had the tools for decades. What’s missing is the will. If your workplace is still using dry-cutting methods, if respirators aren’t fit-tested, if training is a 15-minute video - you’re not just cutting corners. You’re cutting lives.
The question isn’t whether you can afford to prevent these diseases. The question is: can you afford not to?
Can you get silicosis from one-time exposure?
It’s extremely rare. Silicosis usually develops after months or years of repeated exposure. However, acute silicosis can occur after just a few weeks or months of very high exposure - like working in a confined space with no ventilation while cutting engineered stone. This form is aggressive and deadly. Even if you think you only had a short exposure, if you were breathing dust without protection, you should get checked.
Is asbestosis the same as mesothelioma?
No. Asbestosis is scarring of the lung tissue from asbestos fibers. Mesothelioma is a rare, aggressive cancer of the lining of the lungs, heart, or abdomen. Both are caused by asbestos, but they’re different diseases. Mesothelioma has no cure and often appears 20-50 years after exposure. Asbestosis doesn’t cause cancer, but it increases the risk of lung cancer - especially if you smoke.
Are N-95 masks enough for silica or asbestos?
N-95 masks filter 95% of particles, but they’re not always sufficient. Silica and asbestos particles are often smaller than 0.3 microns, and N-95s aren’t designed for oily environments or long-term use. P-100 respirators filter 99.97% of particles, including oil-based ones, and are the recommended standard for these hazards. If you’re doing demolition, cutting stone, or removing insulation, P-100 is the minimum.
Can you test for silicosis or asbestosis before symptoms appear?
Yes. Spirometry - a simple breathing test - can detect early lung function decline before you feel short of breath. Chest X-rays and CT scans can show scarring years before symptoms. The American Thoracic Society recommends baseline testing when exposure starts and repeat testing every 5 years. For high-risk workers, annual testing is advised. Early detection doesn’t reverse damage, but it stops it from getting worse.
What should I do if I worked with asbestos or silica in the past?
Talk to your doctor. Tell them your work history - even if it was decades ago. Get a spirometry test and a chest X-ray. Quit smoking if you haven’t already. There’s no screening test that guarantees you’re safe, but early monitoring gives you the best chance to manage any changes. Don’t wait for symptoms. By the time you feel them, the damage is often advanced.
Is it safe to live in a house with asbestos?
If asbestos materials are intact and undisturbed - like old pipe insulation or floor tiles - they generally don’t pose a risk. The danger comes when they’re damaged, drilled, sanded, or removed. If you’re planning renovations, hire a licensed asbestos abatement professional. Never try to remove it yourself. Air testing can confirm if fibers are present, but the safest approach is to leave it alone unless renovation requires removal.
What Comes Next?
If you’re a worker: ask for a respirator fit test today. If your employer doesn’t offer one, contact OSHA’s whistleblower hotline. Your lungs are worth it.
If you’re an employer: audit your safety practices. Are you using wet methods? Are respirators being tested? Are workers trained? If you’re unsure, use NIOSH’s Prevent eTool - it’s free and built for your industry.
If you’re a policymaker, union rep, or safety officer: push for mandatory health surveillance. Push for stricter enforcement. Push for better tools. The technology exists. The science is clear. The only thing missing is the commitment.
Occupational lung diseases don’t happen by accident. They happen because we let them.