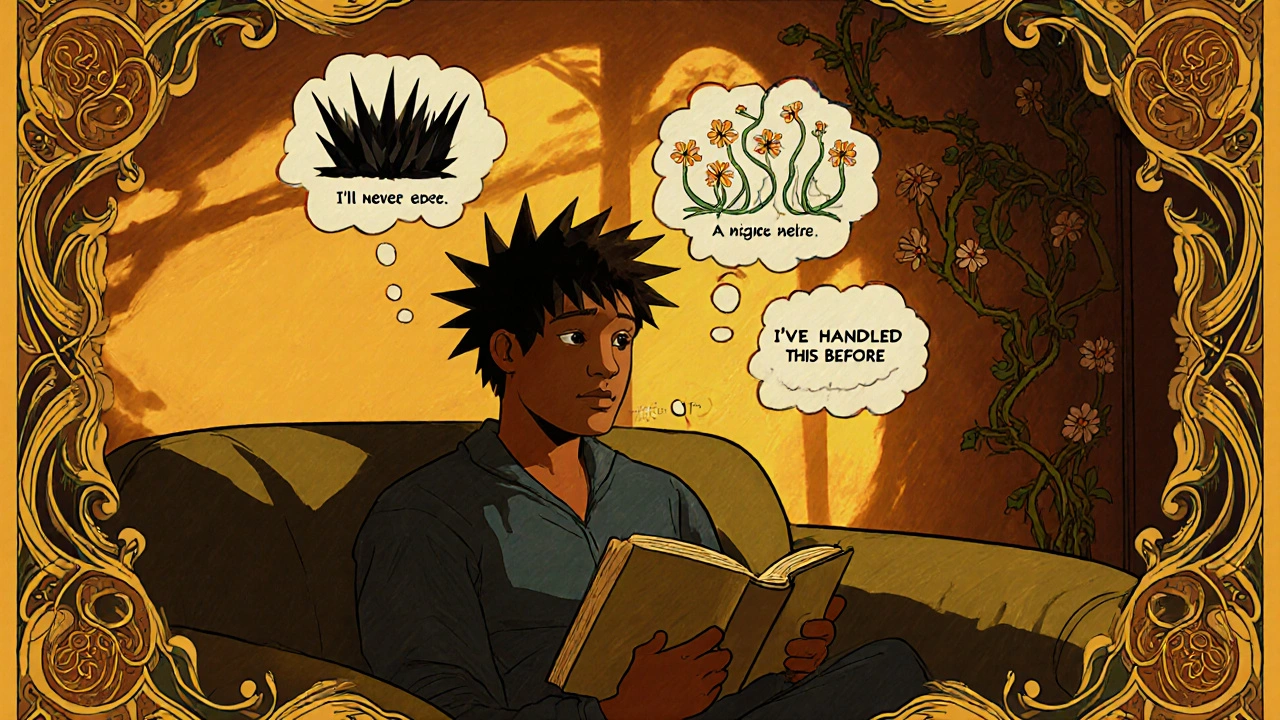
When pain sticks around, it doesn’t just hurt your body-it starts hijacking your mind. You might find yourself thinking, “This will never get better,” or “I can’t handle this anymore,” or even “Something terrible is happening inside me.” These aren’t just bad thoughts. They’re signs of something called pain catastrophizing-a mental pattern that makes pain feel worse, last longer, and steal more from your life than the pain alone ever could.
What Is Pain Catastrophizing?
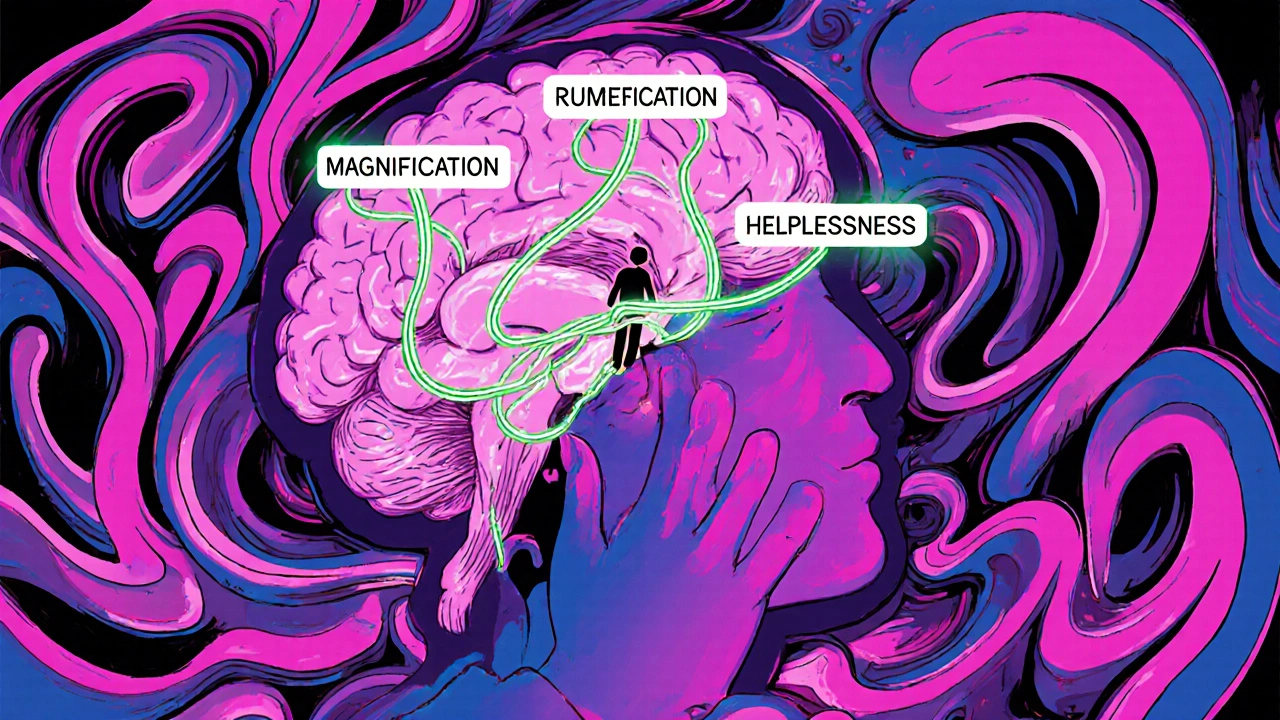
Pain catastrophizing isn’t being dramatic. It’s a real, measurable psychological response that shows up in three ways: rumination (can’t stop thinking about the pain), magnification (believing the pain is way worse than it is), and helplessness (feeling like you have no control). Research from the University of Montreal in the 1990s created the Pain Catastrophizing Scale (PCS) to measure this, and it’s now used worldwide. A score of 30 or higher on the 52-point scale means you’re experiencing clinically significant catastrophizing. It’s not just in your head-it shows up in your brain. Neuroimaging studies show that when someone catastrophizes, areas linked to threat detection and emotion regulation light up like a fire alarm. The more you ruminate on pain, the more your brain amplifies it. This isn’t weakness. It’s a learned response that your nervous system has turned into a habit.Why CBT Works When Other Things Don’t
Painkillers help with the physical sensation, but they don’t touch the mental spiral. Physical therapy might improve movement, but if you’re terrified of moving because you believe it’ll wreck you, you’ll stay stuck. That’s where Cognitive Behavioral Therapy (CBT) steps in-not to deny the pain, but to change how you relate to it. A 2023 review by the International Association for the Study of Pain found that CBT was the only treatment that consistently reduced pain catastrophizing when compared to other therapies. In targeted studies, CBT had nearly double the effect size of other interventions. Even better? When CBT was combined with gentle movement or exercise, the results jumped even higher. People didn’t just feel less distressed-they moved more, slept better, and returned to daily activities they’d given up on. Unlike talk therapy that just explores feelings, CBT gives you tools. It’s practical. It’s structured. And it’s backed by data from thousands of patients, including veterans with chronic pain and people with fibromyalgia, back pain, and arthritis.The Three CBT Tools That Actually Work
You don’t need to be a therapist to use these. These are the same techniques taught in clinics across Australia, the U.S., and Europe.- Self-Monitoring: Start a simple log. Each time pain flares, write down: What happened right before? What thought popped up? How did your body react? You’re not trying to fix it yet-just notice. For example: “Reaching for a coffee mug → ‘This will ruin my shoulder forever’ → Shoulders tightened, heart raced, stopped moving.” Over time, you’ll start seeing patterns.
- Cognitive Restructuring: Once you spot the thought, ask: “Is this thought helping me, or just making things worse?” Then challenge it. Instead of “I’ll never be able to walk again,” try “I’m having a lot of pain today, but I’ve had days like this before, and I still got through them.” This isn’t positive thinking. It’s realistic thinking. You’re replacing fear-based predictions with evidence-based observations.
- Behavioral Activation: Catastrophizing leads to avoidance. Avoidance leads to stiffness, weakness, and more pain. CBT gently pushes you back into life-even in tiny steps. If you stopped gardening because you feared pain, start with 5 minutes. If you stopped socializing, text one friend. Movement doesn’t have to be intense. It just has to be consistent. The goal isn’t to eliminate pain-it’s to stop letting pain decide your life.
Real People, Real Results
A 45-year-old woman in Melbourne with fibromyalgia started CBT with a PCS score of 42-severe catastrophizing. After 12 weeks, her score dropped to 18. Her pain intensity fell by half. She went from working 1 day a week to part-time. She started walking her dog again. She didn’t become pain-free. But she became powerful over her response to pain. On Reddit’s chronic pain forums, 78% of users who stuck with CBT for 8-12 weeks reported a major drop in emotional distress. One user wrote: “I finally realized I wasn’t being weak-I was stuck in a thought loop. CBT gave me the off-ramp.” But it’s not easy. Some people quit because they don’t see quick results. Others say: “When my pain is at an 8, I’m too tired to think clearly.” That’s normal. CBT isn’t about being perfect. It’s about showing up, even when it’s hard. One session a week, 10 minutes of journaling, one small step forward-that’s enough.When CBT Might Not Be Enough
CBT works best when pain is the main problem, not the symptom of something else. If someone is dealing with severe depression, untreated trauma, or active substance use, CBT for pain alone won’t fix it. Those issues need to be addressed first. Pain catastrophizing often rides on top of other mental health challenges. It’s like trying to patch a leaky roof while the whole house is flooding. Also, CBT requires mental energy. If you’re exhausted from sleepless nights or constant discomfort, the idea of “thinking differently” can feel impossible. That’s why some clinics now offer shorter, app-based CBT modules. Apps like Curable and PainScale give you bite-sized exercises you can do while lying down or waiting for a bus. They’re not replacements for therapy-but they’re lifelines for people who can’t make it to weekly sessions.
What’s Next for Pain Catastrophizing Treatment
The future is getting smarter. The U.S. Veterans Health Administration is rolling out a digital dashboard that tracks pain catastrophizing in real time across 170 medical centers. In clinical trials, patients using these tools saw a 32% drop in catastrophizing scores in just 10 weeks. Researchers are also testing “micro-interventions”-short audio prompts sent to your phone when you log high pain or stress. Imagine getting a 90-second voice message saying: “You’re having a catastrophizing moment. Breathe. This feeling will pass. You’ve handled this before.” These aren’t sci-fi. They’re being tested in labs right now. But the core idea won’t change: pain is physical. Suffering is mental. And you have more control over the second than you think.How to Get Started
You don’t need a referral to begin. Start here:- Take the free Pain Catastrophizing Scale (PCS) online-it’s 13 questions, takes 3 minutes. (Search: “Pain Catastrophizing Scale PDF”)
- If your score is 30+, consider talking to a psychologist who specializes in chronic pain.
- Ask your GP for a Mental Health Treatment Plan. In Australia, you can get up to 10 subsidized sessions with a psychologist.
- Try one free CBT app: Curable, PainScale, or This Way Up (offered by St Vincent’s Hospital).
- Start a 5-minute daily journal: Write one thought you had about your pain today. Then write one fact that contradicts it.
Is pain catastrophizing the same as being anxious about pain?
It’s related, but not the same. Anxiety about pain is fear of future pain. Catastrophizing includes that fear, but also rumination (replaying pain in your head) and helplessness (believing you can’t cope). Someone can be anxious without catastrophizing-but if you’re catastrophizing, you’re definitely anxious. CBT targets all three parts.
Can I do CBT for pain catastrophizing on my own?
Yes, but with limits. Many people successfully use apps, workbooks, and online programs. But if your pain is severe, your thoughts feel uncontrollable, or you’ve tried before and failed, working with a trained psychologist increases your chances. Think of it like learning to swim: you can practice alone, but a coach helps you avoid bad habits and stay safe.
How long does it take to see results from CBT for pain catastrophizing?
Most people start noticing shifts in 3-4 weeks-like catching a catastrophic thought before it spirals. Meaningful change-like less distress, better sleep, or returning to activities-usually takes 8-12 weeks. It’s not magic. It’s practice. Think of it like building muscle: small efforts, repeated over time, lead to real strength.
Does CBT mean I’m being told my pain isn’t real?
Absolutely not. CBT doesn’t deny your pain. It acknowledges it fully. What it challenges is the story your mind adds to the pain-the “this will never end” or “I’m broken” narrative. Your pain is real. The suffering that comes from believing you can’t handle it? That’s what CBT helps you reduce.
What if I can’t afford therapy?
There are free or low-cost options. In Australia, Medicare covers up to 10 psychology sessions per year with a Mental Health Treatment Plan. Community health centers often offer sliding-scale fees. Apps like This Way Up and Curable have free versions. Libraries sometimes host pain management workshops. You don’t need a private therapist to start changing how you respond to pain.
akhilesh jha
Interesting breakdown. I’ve been living with chronic back pain for eight years, and I never realized how much my mind was turning every twinge into a catastrophe. The part about neuroimaging lighting up like a fire alarm-that hit me. I didn’t know it was biological, not just ‘being dramatic.’
Natashia Luu
While the clinical data is compelling, one must question the institutionalization of psychological frameworks in pain management. The medical-industrial complex has long preferred cognitive interventions over structural solutions-like access to care, socioeconomic support, or environmental adjustments. This is not healing. It’s adaptation to broken systems.
Victoria Stanley
As someone who’s guided dozens of chronic pain patients through CBT, I can say this: the three tools listed here are the real deal. Self-monitoring is the foundation-people underestimate how powerful simply naming the thought is. It breaks the autopilot. And behavioral activation? Even 5 minutes of movement rewire the brain’s fear response. You don’t need to be ‘fixed.’ You just need to show up.
Andy Louis-Charles
CBT apps are a game-changer. I use Curable every morning while my coffee brews. 90 seconds of guided breathing + one thought challenge. No pressure. No guilt. Just a tiny reset. And yeah, I use emojis 😊 sometimes. It helps me stay consistent.
Douglas cardoza
Man, I tried this last year. Didn’t work for me. Too much thinking when I just wanted to feel better. I’m not gonna sit there writing journals when my leg’s screaming. I need a pill or a shot. Not a lecture.
Adam Hainsfurther
I’m from Nigeria originally, now living in Texas. Here, pain is either ignored or overmedicated. No middle ground. This article bridges that gap. In my culture, we say ‘suffer in silence.’ But silence doesn’t heal-it just buries the pain deeper. This approach? It’s the first thing I’ve seen that respects the body and the mind equally.
Rachael Gallagher
CBT is just corporate brainwashing disguised as therapy. They don’t want you cured-they want you docile. Keep you working while the system ignores your trauma. You think your pain is ‘in your head’? No. It’s in your soul. And they want you to think it’s just your thoughts.
steven patiño palacio
Victoria’s comment resonates deeply. I’ve seen patients who resisted CBT because they felt blamed. But the key is framing: this isn’t about fixing you. It’s about freeing you from the mental prison your pain has built. One client, a retired firefighter, started with 45 on the PCS. After 10 weeks? 14. He started coaching little league again. Not because the pain vanished. Because he stopped letting it dictate his life.
stephanie Hill
Have you noticed how every ‘evidence-based’ pain solution comes from big pharma-funded studies? CBT is convenient-it’s cheap, non-invasive, and keeps people off opioids. But what if the real issue is environmental toxins? Or glyphosate in our food? Or the fact that no one checks your vitamin D? They don’t want you asking those questions.
Akash Chopda
My pain is real. My thoughts are real. The system is broken. No one helps. Just apps and journals. I give up
Jeff Hicken
Wow this is a lot of words for ‘just think happy thoughts.’ I read like half of it and my back hurt more just from trying to focus. Also typo in ‘catastrophizing’ lol. And why are there so many questions at the bottom? Who writes like this?
Vineeta Puri
To Akash and others who feel hopeless: your pain is valid, and your exhaustion is real. CBT is not a cure-all, nor is it a demand for perfection. It’s a quiet rebellion against the idea that you must suffer in silence. Start with one sentence in a journal. One deep breath. One small movement. You are not failing. You are still here-and that is strength.