Psoriasis isn’t just a rash. It’s your immune system attacking your own skin-turning healthy skin cells into thick, scaly plaques in a matter of days. For millions of people, flare-ups don’t come out of nowhere. They’re triggered by things you can see, feel, and sometimes control. The biggest culprits? Stress, infections, and a broken skin barrier. Understanding how these three factors work together isn’t just helpful-it’s often the difference between constant flares and long stretches of relief.
Stress Doesn’t Just Make You Tense-It Ignites Psoriasis
Think stress is just a mental thing? Think again. When you’re overwhelmed-whether from grief, work pressure, or even a big life change like moving or a new job-your body floods your system with cortisol and other inflammatory chemicals. These don’t just make you feel anxious. They directly activate the immune cells that drive psoriasis.
Research shows that up to 70% of people with psoriasis link their worst flares to stressful events. One woman in Melbourne lost her mother and saw her plaque psoriasis spread from small patches on her elbows to covering 30% of her body in just three months. That’s not coincidence. Stress doesn’t cause psoriasis in someone who’s genetically clear, but in those with the genes, it’s like lighting a match near gasoline.
And here’s the cruel twist: psoriasis itself causes stress. Worrying about how your skin looks, avoiding social situations, or feeling embarrassed can spiral into anxiety and depression-which then triggers more flares. It’s a loop. Breaking it isn’t about ignoring stress. It’s about managing it. Studies show that 20 minutes of daily mindfulness meditation can lower cortisol by 25% in eight weeks. Regular walking, yoga, or even talking to a therapist can cut flare frequency by 30% or more. You don’t need to be zen. You just need to build habits that give your nervous system a break.
Infections Are Silent Triggers-Even Common Colds Can Spark Flares
When you get a sore throat, a bad cold, or even the flu, your immune system goes into overdrive. That’s normal. But for someone with psoriasis, that overdrive doesn’t shut off. It turns on the wrong cells. Specifically, strep throat is a known trigger for guttate psoriasis-a type that looks like small, drop-like spots, often appearing suddenly in kids and young adults. Even COVID-19 has been linked to new-onset psoriasis or sudden worsening in existing cases.
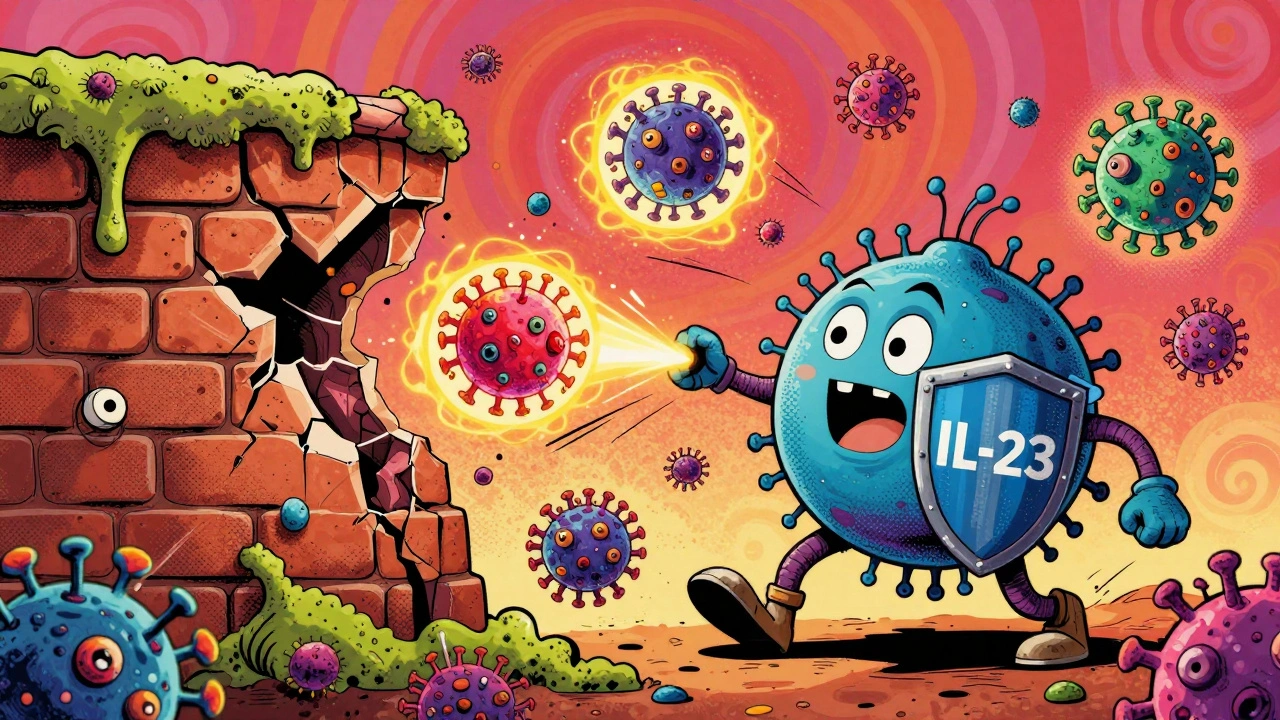
The science behind this is precise. Viruses activate a sensor in your skin cells called RIG-I, which then signals immune cells to release IL-23, a key driver of psoriasis inflammation. Bacterial infections do the same thing. Your body’s attempt to fight off the infection accidentally wakes up the autoimmune response hiding in your skin.
That’s why prevention matters. Simple steps like washing your hands often, getting your annual flu shot, and avoiding close contact with sick people can reduce infection-triggered flares by up to 35%. If you notice a flare starting after a cold or sore throat, don’t wait. Talk to your dermatologist. Early treatment can stop it from spreading. And if you’ve had repeated infection flares, your doctor might suggest checking for hidden infections-like lingering strep in your tonsils-that you didn’t even know you had.
Your Skin Barrier Isn’t Just a Layer-It’s Your First Line of Defense
Imagine your skin like a brick wall. The bricks are skin cells. The mortar is the natural oils and proteins that hold them together. In psoriasis, that mortar is weak. The LCE gene family, which helps build this barrier, is often faulty in people with psoriasis. When the barrier breaks down, moisture escapes, germs get in, and your skin becomes a breeding ground for inflammation.
This isn’t just about dryness. It’s a cycle: broken barrier → bacteria overgrowth → immune activation → more inflammation → worse barrier. Studies on mice with damaged skin showed that when researchers reduced bacteria with topical antibiotics, psoriasis-like symptoms disappeared. The same pattern happens in humans.
So how do you fix it? You don’t need fancy products. You need the right basics. Use fragrance-free moisturizers with ceramides, hyaluronic acid, or glycerin-applied at least twice a day, right after your shower. Avoid soaps with a high pH (above 5.5). They strip away your natural oils. Look for labels that say “pH-balanced” or “for sensitive skin.”
Humidity matters too. In Melbourne’s winter, indoor heating drops humidity to 20%. Your skin suffers. A simple humidifier in your bedroom, keeping levels between 40-60%, can make a huge difference. And never scratch. Even a tiny insect bite or sunburn can trigger the Koebner phenomenon-where psoriasis forms exactly where your skin was injured. Use cool compresses, not your nails, to soothe itchy spots.
How These Triggers Work Together
Stress, infection, and skin barrier damage don’t act alone. They feed each other. Stress weakens your skin barrier. A weakened barrier makes it easier for bacteria to invade, triggering infection. Infection spikes inflammation, which increases stress. It’s a feedback loop that keeps psoriasis alive.
That’s why treating just one part rarely works long-term. If you manage stress but keep using harsh soaps, your barrier stays broken. If you moisturize perfectly but get frequent colds, flares will keep coming. The key is attacking all three at once.
Here’s what a real-world plan looks like:
- Morning: Apply ceramide moisturizer after washing with a gentle cleanser
- Afternoon: Use a humidifier if indoors; avoid direct wind or dry heat
- Evening: Wash hands before bed; apply thick ointment to flares
- Weekly: 3 sessions of 20-minute mindfulness or light exercise
- Seasonally: Get flu shot; check for sore throats or lingering infections
People who follow this kind of routine report 40-60% fewer flares over six months. It’s not a cure. But it’s control.

What You Can Do Today to Reduce Flares
You don’t need to overhaul your life. Start small.
- Switch to a fragrance-free, soap-free cleanser today. Look for ingredients like sodium lauroyl sarcosinate or cocamidopropyl betaine.
- Keep a small jar of ceramide cream by your sink and apply it every time you wash your hands.
- Set a daily 10-minute alarm for deep breathing. Breathe in for 4 counts, hold for 4, out for 6. Do it before bed.
- Write down every flare and what happened 2-3 days before. Was it stress? A cold? A new detergent? Patterns will show up.
- Call your doctor if you’ve had three colds in six months. You might need a deeper check for hidden triggers.
The goal isn’t perfection. It’s awareness. The more you understand your triggers, the less power they have over you.
What’s Next for Psoriasis Treatment?
Science is moving fast. New biologic drugs target the exact immune pathways activated by stress and infection-like IL-23 inhibitors. In trials, 89% of patients saw 90% improvement in their plaques within four months. But these are expensive and not for everyone.
Even more exciting? Wearable tech. Researchers are testing smart patches that track stress hormones and skin hydration in real time. Within five years, AI apps might predict your next flare before it starts-based on your sleep, stress levels, and even local weather. That’s the future.
For now, the best tool you have is knowledge. Know your triggers. Protect your skin. Manage your stress. Treat infections early. You’re not powerless. You’re just learning how your body works.
Can stress really cause psoriasis to get worse?
Yes. Stress doesn’t cause psoriasis in someone without the genes, but it’s one of the most powerful triggers for flares in people who already have it. When stressed, your body releases inflammatory chemicals that activate the immune cells responsible for psoriasis. Many patients report flares starting within weeks of major life stress-like losing a loved one or changing jobs. Managing stress through mindfulness, exercise, or therapy can reduce flare frequency by up to 30%.
Can a cold or sore throat trigger psoriasis?
Absolutely. Infections, especially strep throat, are a well-documented trigger for guttate psoriasis, particularly in children and young adults. Viruses and bacteria activate immune sensors in the skin that ramp up IL-23 production, which directly fuels psoriasis inflammation. Even common colds and flu can spark flares. Getting your annual flu shot and practicing good hand hygiene can reduce infection-triggered flares by about 35%.
What’s the best way to repair a damaged skin barrier?
Use fragrance-free, pH-balanced moisturizers with ceramides, hyaluronic acid, or glycerin-applied twice daily, right after showering. Avoid harsh soaps, hot water, and scrubbing. Keep indoor humidity between 40-60%, especially in winter. A humidifier helps. Never scratch-it can trigger new plaques through the Koebner effect. Even minor injuries like bug bites or sunburns can start flares. Cool compresses work better than scratching.
Do I need to avoid certain foods to stop psoriasis flares?
Food isn’t a primary trigger for most people, but some do notice reactions. A 2022 survey found 32% of psoriasis patients linked flares to dairy, 25% to gluten, and 18% to nightshades like tomatoes or peppers. If you suspect food is a trigger, try eliminating one group at a time for 4-6 weeks. Keep a journal. Don’t cut out entire food groups without checking with a dietitian-nutrition matters for overall immune health.
Can psoriasis be cured by fixing these triggers?
No-psoriasis is a chronic autoimmune condition, so there’s no cure yet. But managing triggers can dramatically reduce flare frequency and severity. Many people go months or even years without flares when they protect their skin barrier, manage stress, and prevent infections. The goal isn’t perfection. It’s control. With the right routine, you can live with psoriasis without letting it control your life.
If you’ve been struggling with flares, start with one change today. Swap your soap. Apply moisturizer after washing your hands. Breathe deeply for five minutes before bed. Small steps add up. Your skin will thank you.

parth pandya
man i been dealin w/ psoriasis since i was 16 and stress is THE worst for me. work deadlines? boom, elbows flare up. family drama? whole back turns into a map of scales. i tried meditating but i just end up stressin about not meditating right lol. the moisturizer thing though? ceramides saved my life. switched to ceraVe and no more burning when i shower. also, stop usin hot water. it feels good but it’s like pourin gasoline on fire.
Albert Essel
This is one of the most well-researched and empathetic explanations of psoriasis triggers I’ve encountered. The connection between stress-induced cortisol and IL-23 activation is not only scientifically accurate but also presented in a way that empowers rather than overwhelms. I especially appreciate the emphasis on the skin barrier’s structural integrity-too many focus solely on symptoms and neglect the foundational biology. Thank you for this.
Gavin Boyne
So let me get this straight-we’re told to meditate, moisturize, avoid colds, stop scratching, use humidifiers, eat less dairy, and now we’re supposed to buy smart patches that track our stress hormones like we’re NASA astronauts preparing for Mars? Meanwhile, my insurance won’t cover a $20 bottle of ceramide cream but will pay for a $12,000 biologic. Yeah, I’ll just keep scratching and pretending I’m not a walking autoimmune experiment. 😌
Rashi Taliyan
OH MY GOD. I JUST REALIZED MY FLARES STARTED AFTER I MOVED TO A NEW APARTMENT WITH NO HUMIDIFIER. IT WAS SO DRY I COULD HEAR MY SKIN CRACKING AT NIGHT 😭 I GOT A HUMIDIFIER LAST WEEK AND MY ELBOWS ARE ACTUALLY SMOOTH?? I’M CRYING. I THOUGHT I WAS JUST BROKEN. THIS ARTICLE IS A GIFT. THANK YOU. I’M GOING TO BUY CERAMIDE CREAM RIGHT NOW. I’M NOT ASKING FOR PERMISSION ANYMORE.
Kara Bysterbusch
While the physiological mechanisms elucidated herein are both compelling and evidence-based, I would respectfully propose an additional consideration: the sociocultural dimension of psoriasis management. In many communities, particularly those with limited access to dermatological care, the burden of self-management is disproportionately shouldered by individuals without adequate resources. The suggestion to ‘apply moisturizer twice daily’ assumes not only availability but also temporal and economic privilege. A more holistic approach would integrate systemic advocacy with personal strategy.
Rashmin Patel
Okay but can we talk about how everyone’s acting like this is some new revelation?? I’ve been telling my cousins in Delhi for years: stop using Lifebuoy soap, it’s pH 9.8 and your skin is NOT a toilet. And yes, stress makes it worse-my aunt’s psoriasis exploded after her husband left her, and she didn’t even know why. She thought it was ‘bad luck’. No, it was cortisol + dry air + scratching while watching TV at 2am. 🤦♀️ I started giving everyone in my family ceramide cream for birthdays now. It’s cheaper than therapy and actually works. Also, humidifier = non-negotiable. If you live in a place where winter feels like a desert, you owe it to your skin to buy one. I bought mine off Amazon for $30. Your skin will hug you back.
sagar bhute
This is just a glorified wellness blog. You think meditation fixes autoimmune disease? You think moisturizer stops your immune system from going rogue? Psoriasis is genetic. It’s not about your ‘habits’ or your ‘stress levels’. You’re just giving false hope to people who are already suffering. Stop pretending this is controllable. It’s not. You’re just making people feel guilty for not being ‘perfect’ enough.
Cindy Lopez
Interesting. But you mention ‘strep throat’ as a trigger without citing the original study. Also, ‘35% reduction’ from handwashing? That’s a vague statistic. Where’s the source? And why no mention of the microbiome’s role in barrier repair? This reads like a marketing pamphlet disguised as medical advice.
James Kerr
My dude, I’ve had this for 12 years. The moisturizer + humidifier + handwashing combo? Game changer. I don’t meditate, but I do sit outside for 10 mins every morning with my coffee. That’s my ‘zen’. And yeah, I still get flares. But now they’re tiny. Not full-body panic mode. Just one patch. I’m not cured. But I’m not crying in the shower anymore. 🙌