Bipolar Antidepressant Risk Calculator
This tool helps assess your risk of mania, hypomania, or rapid cycling when taking antidepressants for bipolar depression. Based on the article "Antidepressants and Bipolar Disorder: When Treatment Risks Outweigh Benefits".
For someone living with bipolar disorder, finding relief from deep depression can feel like the only thing that matters. But what if the very medication meant to help - an antidepressant - could push you into mania, rapid cycling, or even a mixed state where despair and agitation collide? This isn’t a rare accident. It’s a well-documented risk, and one that many doctors still ignore.
Why Antidepressants Are a Double-Edged Sword in Bipolar Disorder
Antidepressants work by boosting serotonin, norepinephrine, or dopamine in the brain. That’s great for unipolar depression - where the brain just lacks mood-lifting chemicals. But in bipolar disorder, the brain isn’t just low; it’s unstable. The same chemicals that lift you out of depression can flip the switch into mania. Studies show that about 12% of people with bipolar disorder who take antidepressants will experience a switch into mania or hypomania - even when they’re taking a mood stabilizer. That number jumps to 31% in real-world, long-term use. For comparison, about 10.7% of people on mood stabilizers alone will switch naturally. That means antidepressants aren’t preventing switches - they’re adding to them. The risk isn’t the same for everyone. People with Bipolar I, a history of prior antidepressant-induced mania, or rapid cycling (four or more mood episodes a year) are at highest risk. Those with mixed features - depression with agitation, irritability, or racing thoughts - are especially vulnerable. In these cases, antidepressant switch risk can exceed 30%.What the Guidelines Actually Say (And What Doctors Still Do)
The International Society for Bipolar Disorders (ISBD) and the American Psychiatric Association (APA) agree: antidepressants should not be first-line treatment for bipolar depression. Instead, they recommend FDA-approved options like quetiapine, lurasidone, cariprazine, or the combination of olanzapine and fluoxetine. These drugs have proven response rates of 50% or higher - with switch risks under 5%. Yet, in clinical practice, about 50% to 80% of people with bipolar disorder still get antidepressants. In community clinics, that number hits 80%. Why? Because they’re familiar. Because patients ask for them. Because doctors don’t always have time to learn new protocols. The gap between guidelines and practice is staggering. Only 30% of community psychiatrists follow ISBD recommendations. In academic centers, it’s 65%. That means most people with bipolar disorder are being treated with outdated, risky methods.Which Antidepressants Are Riskiest?
Not all antidepressants are created equal. Tricyclics - older drugs like amitriptyline - carry the highest switch risk: 15% to 25%. SNRIs like venlafaxine aren’t much better. SSRIs - like sertraline, fluoxetine, or escitalopram - are often seen as safer. They carry a lower risk: around 8% to 10%. Bupropion (Wellbutrin) is sometimes used because it doesn’t strongly affect serotonin. But even these aren’t risk-free. The problem isn’t just the drug class. It’s how they’re used. Monotherapy - taking an antidepressant alone - is dangerous. Even when paired with a mood stabilizer, long-term use increases the chance of rapid cycling. One study found people on antidepressants for more than 24 weeks had a 37% higher risk of recurring episodes.The Illusion of Quick Relief
One reason antidepressants are still used is speed. They can lift mood in 2 to 4 weeks. Mood stabilizers like lithium or lamotrigine often take 6 to 8 weeks to show full effect. For someone in deep despair, that wait feels unbearable. But here’s the catch: the benefit is minimal. The number needed to treat (NNT) for antidepressants in bipolar depression is 29.4. That means you’d need to give antidepressants to nearly 30 people to help one person feel better. Compare that to unipolar depression, where the NNT is 6 to 8. In bipolar disorder, antidepressants barely outperform placebo. Meanwhile, the number needed to harm (NNH) for a mood switch is about 200. That sounds low - until you realize that 200 people means 1 person gets hospitalized, loses a job, or ends up in the ER because of mania. That’s not a trade-off worth making.
When Might Antidepressants Be Justified?
There are rare cases where antidepressants might be considered - but only under strict conditions:- Severe, treatment-resistant depression that hasn’t responded to at least two FDA-approved bipolar depression treatments
- No history of antidepressant-induced mania
- No rapid cycling or mixed features
- Used only as a short-term add-on to a mood stabilizer or atypical antipsychotic
- Weekly monitoring for the first month for any sign of energy surge, reduced sleep, or impulsivity
- Discontinued within 8 to 12 weeks, even if the person feels better
What Happens When You Don’t Stop
The biggest mistake? Keeping antidepressants too long. In 65% of community cases, patients stay on them for months or years. That’s not treatment - it’s destabilization. Long-term use increases episode frequency by 1.7 times. It can turn a stable person into a chronic rollercoaster. Some patients report feeling “wired” or “on edge” even when not manic - a sign their brain is becoming sensitized to mood swings. And here’s the cruel irony: antidepressants can interfere with the effectiveness of mood stabilizers. One study showed lithium worked less well in people also taking SSRIs. The brain’s chemistry gets tangled.Real Stories, Real Consequences
Patient experiences are split. Some say, “SSRIs saved my life - I could finally work again.” Others say, “One pill sent me into a three-week mania. I lost my apartment. I had to be hospitalized.” The STEP-BD study found no big difference in remission rates between people taking antidepressants and those on mood stabilizers alone. But the emotional toll? That’s harder to measure. One woman in a support group described waking up after a manic episode with her credit cards maxed out and no memory of how she got there. “I thought the antidepressant was helping,” she said. “It was just making me lose control.”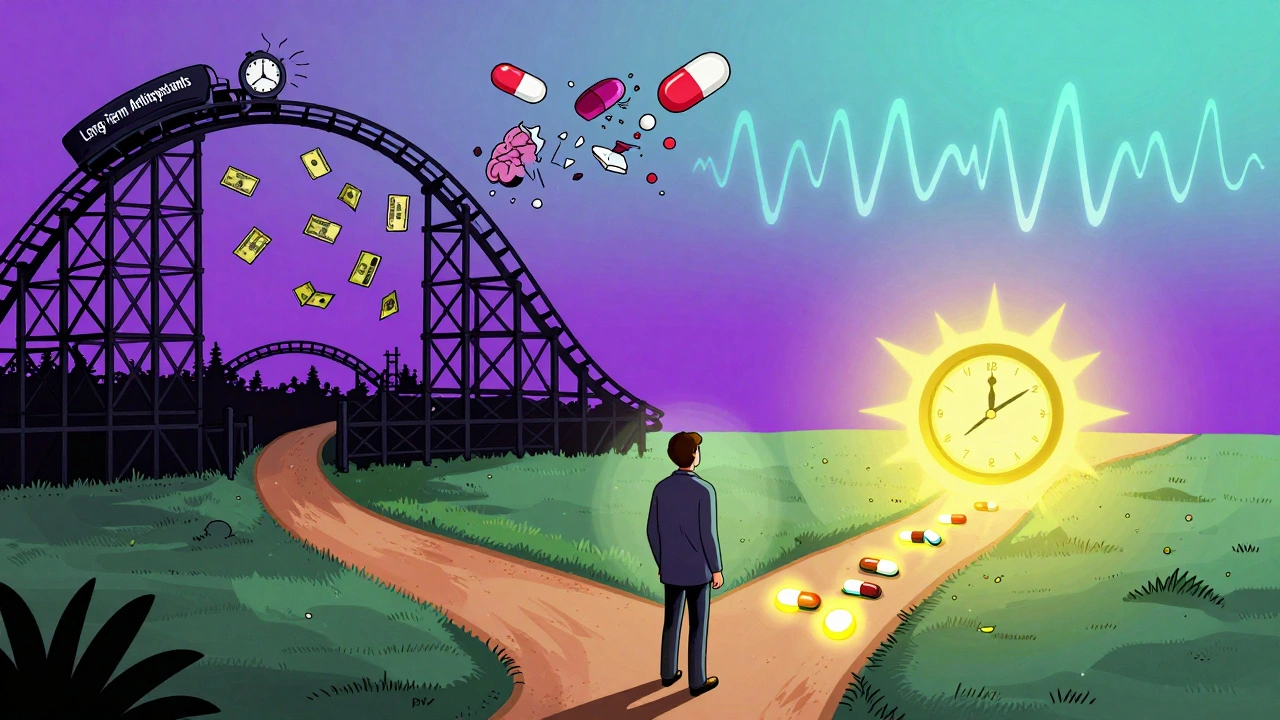
The Future: Better Options Are Here
The good news? We don’t have to keep using risky tools. Since 2006, the FDA has approved four non-antidepressant treatments for bipolar depression. Quetiapine, lurasidone, cariprazine, and olanzapine-fluoxetine are all proven to work - with far fewer risks. Newer options are coming fast. Esketamine nasal spray showed a 52% response rate in bipolar depression with only 3.1% switch risk in a 2023 trial. That’s better than any antidepressant. Research is also moving toward precision medicine. Scientists are studying genetic markers like the 5-HTTLPR gene variant. People with the LL genotype have over three times the risk of switching on antidepressants. In the near future, a simple blood test might tell you whether an antidepressant is safe for you - or a recipe for disaster.What You Should Do If You’re on Antidepressants
If you have bipolar disorder and are taking an antidepressant:- Ask your doctor: “Is this FDA-approved for bipolar depression?” If not, why are we using it?
- Ask: “Have I ever had a manic episode triggered by medication?” If yes, this drug is likely unsafe.
- Track your sleep, energy, and irritability daily. A sudden drop in sleep needs or increased spending, talking fast, or risky behavior are red flags.
- Request a review of your treatment plan every 8 weeks. If you’ve been on it longer than 12 weeks, ask about tapering off.
- Ask about alternatives: quetiapine, lurasidone, or lamotrigine. These are safer and just as effective.
Why This Matters Beyond the Prescription
This isn’t just about one drug. It’s about how we treat mental illness. We’ve spent decades treating bipolar depression like unipolar depression - because it looks the same. But the brain doesn’t care how it looks. It cares how it functions. Using antidepressants in bipolar disorder is like putting a bandage on a broken bone. It hides the pain - but makes the injury worse. The science is clear. The guidelines are clear. The risks are real. The better options are here. It’s time to stop treating bipolar depression with tools designed for a different illness.Can antidepressants cause mania in people with bipolar disorder?
Yes. Antidepressants can trigger manic or hypomanic episodes in people with bipolar disorder. Studies show about 12% of patients experience a switch into mania when taking antidepressants, and that risk rises to 31% in real-world settings. The risk is highest with tricyclics and SNRIs, but even SSRIs carry a measurable danger - especially in those with Bipolar I, rapid cycling, or mixed features.
Are there safer alternatives to antidepressants for bipolar depression?
Yes. Four FDA-approved treatments specifically for bipolar depression are safer and more effective: quetiapine (Seroquel), lurasidone (Latuda), cariprazine (Vraylar), and the combination of olanzapine and fluoxetine (Symbyax). These drugs have response rates of 48% to 60% and switch risks under 5%. They’re now considered first-line treatments by major psychiatric guidelines.
How long should someone stay on an antidepressant if they have bipolar disorder?
If an antidepressant is used at all, it should be short-term - no longer than 8 to 12 weeks - and only as an add-on to a mood stabilizer or atypical antipsychotic. Long-term use increases the risk of rapid cycling, more frequent episodes, and reduced effectiveness of mood stabilizers. Most guidelines recommend discontinuing antidepressants after this period, even if the person feels better.
What are the warning signs that an antidepressant is causing mood destabilization?
Warning signs include reduced need for sleep, increased energy or restlessness, racing thoughts, impulsivity (like reckless spending or risky sex), irritability, or talking much more than usual. These can appear within days or weeks of starting or increasing the dose. If any of these occur, contact your doctor immediately - don’t wait for full mania to develop.
Why do doctors still prescribe antidepressants for bipolar disorder if they’re risky?
Many doctors prescribe them out of habit, patient demand, or lack of familiarity with newer guidelines. Antidepressants are widely known, easy to prescribe, and patients often ask for them because they’ve heard they “help with depression.” But research shows only 30% of community psychiatrists follow current bipolar treatment guidelines. In academic centers, adherence is higher - around 65% - highlighting a major gap between evidence and practice.
Is it safe to take an antidepressant if I have Bipolar II?
It’s still risky. While some experts believe Bipolar II may be slightly less vulnerable to switching, the risk remains. Studies show even in Bipolar II, antidepressants can trigger mania, hypomania, or rapid cycling. The presence of mixed features, prior switch history, or rapid cycling increases danger regardless of subtype. Most guidelines still recommend avoiding antidepressants as first-line treatment, even in Bipolar II.

Katie Allan
It’s terrifying how often doctors treat bipolar depression like regular depression. I’ve seen friends go from barely functional to hospitalized because a doctor prescribed an SSRI without checking their history. The science is clear, but the system isn’t listening. We need better training, not just better drugs.
It’s not about blaming doctors - they’re overworked and under-resourced. But this isn’t just negligence. It’s systemic failure. We keep using tools designed for a different illness because it’s easier than learning new protocols. And the cost? Real lives.
There’s a reason why people with bipolar disorder have higher suicide rates than those with unipolar depression - we’re being treated like broken machines, not complex human brains.
Why is it still considered acceptable to prescribe something with a 30% risk of triggering mania when safer options exist? Because we’ve normalized risk in mental health care. We’ve accepted that some people will get hurt because the system can’t keep up.
But we don’t have to. We have the data. We have the alternatives. We just need the will.
It’s time to stop treating bipolar disorder as if it’s just depression with mood swings. It’s a fundamentally different illness. And we owe it to every person struggling to treat it that way.
Mark Curry
My brother was on an SSRI for 3 years. He didn’t realize he was cycling until he lost his job and his car. Now he’s on lamotrigine and actually sleeping. I wish someone had told us sooner.
It’s not that antidepressants don’t work - it’s that they work too well at making you feel better, until they don’t.
Just don’t stay on them too long. That’s the key.
aditya dixit
There’s a quiet tragedy in how we treat mental illness - we treat symptoms, not systems. Antidepressants are a bandage on a broken spine. We don’t fix the spine. We just numb the pain until the spine collapses.
What if we stopped asking ‘how do we make people feel better?’ and started asking ‘how do we help their brains heal?’
That’s the real shift needed. Not new drugs. New thinking.
And yes - the FDA-approved options are better. But they’re also more expensive, harder to access, and often ignored by insurance. So the problem isn’t just medical. It’s economic.
Until we fix the system that prioritizes profit over care, people will keep getting prescribed what’s cheap and familiar - even if it’s dangerous.
Knowledge is power. But power without access is just a footnote in someone else’s story.
an mo
Let’s be real - antidepressants are a pharmaceutical industry cash cow. They’ve spent billions marketing them as ‘the solution’ for every kind of sadness. Bipolar? Just slap on an SSRI. Done. No need to investigate the root cause or risk of destabilization.
The real scandal? The FDA approved these drugs for bipolar depression only after years of pressure - and even then, most docs don’t know the difference between ‘approved for’ and ‘recommended for.’
It’s not ignorance. It’s profit.
And guess who pays? The people who can’t afford to switch meds. The ones who lose jobs. The ones who end up in ERs.
They’re not patients. They’re revenue streams.
Norene Fulwiler
I’m from a culture where mental health is still whispered about. But when my cousin went from crying all day to sleeping 2 hours and spending $20k in a week after starting Zoloft, we finally got it.
Antidepressants aren’t magic. They’re chemical roulette.
Thank you for saying this out loud. People need to hear it.
Lucy Kavanagh
Why are we letting Big Pharma dictate how we treat mental illness? The same companies that pushed opioids are now pushing antidepressants. They don’t care if you switch into mania - they care if you keep buying.
And don’t even get me started on how the NHS and Medicare refuse to cover quetiapine unless you’ve tried 3 SSRIs first. It’s like they want you to suffer before they’ll help.
This isn’t medicine. It’s corporate control.
Harry Nguyen
Oh wow. Another article saying antidepressants are bad. Shocking. I’m sure the 12% who got mania were just unlucky. Meanwhile, the 88% who got their lives back are just… what? Lying?
Some people need antidepressants. Not everyone has a perfect diagnosis. Not everyone has access to fancy new drugs. Not everyone can wait 8 weeks for lamotrigine to kick in.
Maybe instead of demonizing meds, we should fix the system that makes people choose between no help and risky help.
Also, ‘bandage on a broken bone’? Really? That’s your analogy? Wow. Deep.
Ali Bradshaw
I’ve been on lithium for 7 years. Never touched an antidepressant. I’m stable. I work. I have friends.
But I know people who were on SSRIs for years - and now they’re on 4 meds just to stay level.
It’s not about being scared of meds. It’s about being smart with them.
Don’t start something you don’t know how to stop.
Ada Maklagina
My psychiatrist said ‘try it for 6 weeks’ and never followed up. I didn’t know I was cycling until I got arrested for shoplifting during a hypomanic episode. I was just ‘feeling productive.’
Don’t trust doctors who don’t monitor you.
And track your sleep. Always.
Kylee Gregory
I used to think antidepressants were the answer. Then I saw how they made my sister’s mood swings worse - and how she blamed herself for ‘not being strong enough’ when she crashed after the mania.
It’s not about the drug. It’s about how we talk about mental health.
We treat bipolar disorder like a personal failure instead of a neurological condition.
Maybe if we stopped shaming people for needing help - and started demanding better care - we’d see fewer tragedies.
Not everyone needs to be ‘cured.’ Some just need to be held.
Mellissa Landrum
they told me sertraline was safe for bipolar 2 so i took it for 2 years then i spent 3 months in a hotel room with 12 credit cards and no memory of how i got there
now i take lamotrigine and i can sleep again
doctors dont know shit
ps i hate the word 'switch' its so clinical its dehumanizing
Juliet Morgan
I was told SSRIs were ‘low risk’ for Bipolar II. Turns out ‘low risk’ means ‘you’re the one who gets the 10%.’
After my first mania, I asked my doctor why they didn’t warn me. She said, ‘I didn’t think it would happen to you.’
That’s not medicine. That’s gambling with someone’s life.
Don’t trust ‘low risk.’ Trust data. Trust guidelines. Trust yourself.
William Chin
It is imperative to underscore that the clinical paradigm surrounding the pharmacological management of bipolar depression remains profoundly misaligned with evidence-based standards. The continued utilization of antidepressants as monotherapy or even as adjunctive agents, absent rigorous monitoring and strict temporal limitations, constitutes a significant departure from internationally recognized clinical guidelines. The potential for iatrogenic destabilization is not merely theoretical - it is empirically validated, quantifiable, and ethically untenable. One must therefore advocate for the immediate adoption of FDA-approved mood-stabilizing agents, and eschew the antiquated, placebo-influenced practices that continue to dominate community-based care. The patient’s stability is not negotiable.
Mark Ziegenbein
Look, I get it - the science says antidepressants are risky, but let’s be honest here: if you’ve been depressed for 18 months and your doctor says ‘take this and you’ll feel better in 2 weeks’ - you’re going to take it. You’re not sitting there reading the ISBD guidelines. You’re just trying to get out of bed. And if you do, if you finally feel like yourself again for the first time in years - you’re not going to stop because some study says ‘oh but you might get manic in 6 months.’
That’s not rational. That’s not human. That’s privilege talking.
People don’t have the luxury of waiting 8 weeks for lamotrigine to kick in. They have rent. They have kids. They have jobs they might lose if they don’t show up.
So yes, the guidelines are right. But the system is broken. And until we fix the system - the fact that someone took an SSRI and survived for 5 years without a switch doesn’t make them a statistic. It makes them a person who got lucky.
And maybe - just maybe - that’s the real tragedy.
We don’t need more rules. We need more access. More time. More compassion. Not just better drugs.
Chris Brown
It’s irresponsible to claim antidepressants are universally dangerous. The data is nuanced. Some patients benefit. Some don’t. But to generalize like this is to undermine the very foundation of individualized care. Mental illness is not a one-size-fits-all condition. To dismiss decades of clinical use based on aggregate statistics is to ignore the lived experience of millions who have regained functionality, employment, and relationships through these medications.
The real issue isn’t the drugs - it’s the lack of proper diagnostic rigor. Misdiagnosed unipolar depression is often mistaken for bipolar disorder. And when that happens, antidepressants work beautifully. To blame the medication for the misdiagnosis is not science - it’s scapegoating.
Let’s fix diagnosis before we ban treatment.