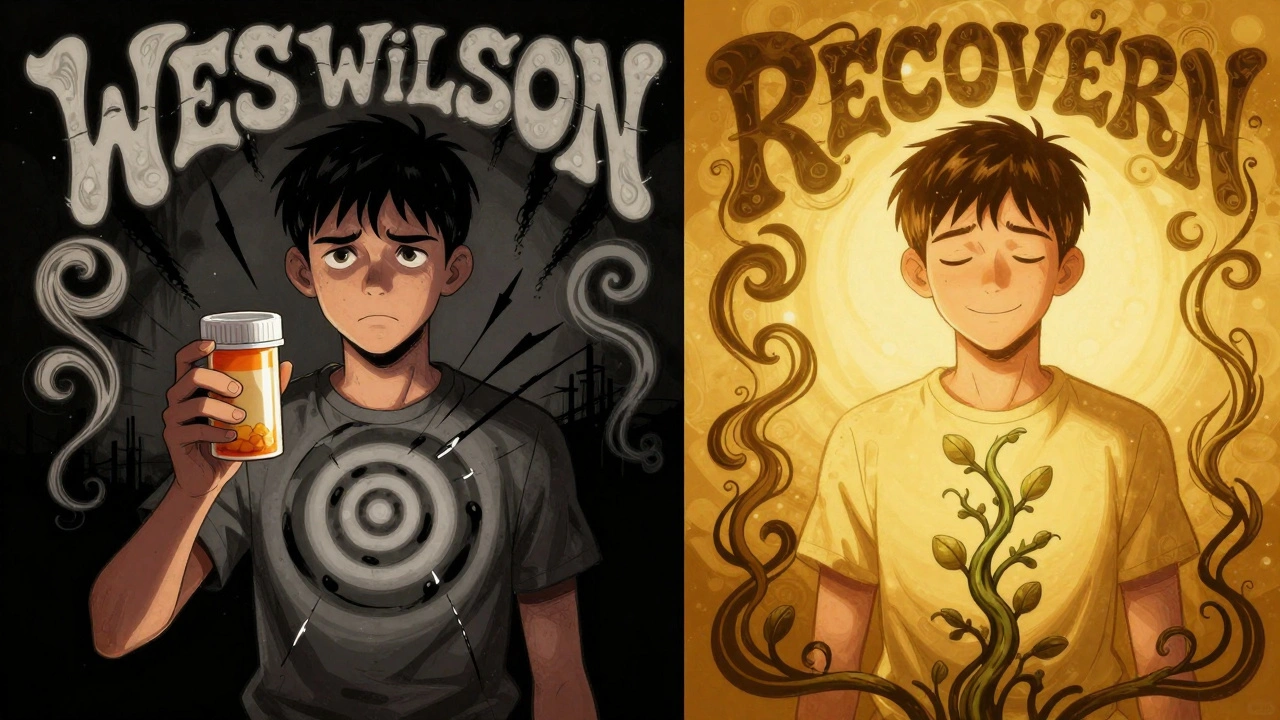
When you start taking an antidepressant, you expect to feel better. But what if the very medicine meant to lift you out of darkness starts to make you think about ending your life? This isn’t a rare scare tactic-it’s a real, documented risk that the U.S. Food and Drug Administration (FDA) flagged with its strongest possible warning: the black box warning.
What Is a Black Box Warning?
A black box warning is the FDA’s most serious alert for prescription drugs. It’s printed in bold, black borders at the very top of the medication’s official prescribing information. It doesn’t mean the drug is dangerous for everyone. It means that for some people, under certain conditions, the risks are real enough that doctors and patients need to pay close attention.For antidepressants, the warning says this: children, adolescents, and young adults up to age 24 may have an increased risk of suicidal thoughts or behaviors when starting treatment. It’s not saying antidepressants cause suicide. It’s saying they might trigger a surge in suicidal thinking during the first few weeks or months-especially before the medicine starts working to lift mood.
This warning wasn’t made up overnight. In 2004, after reviewing data from 24 clinical trials involving over 4,400 young patients, the FDA found that about 4% of kids and teens taking antidepressants showed signs of increased suicidality-like talking about death, making plans, or acting on impulses-compared to 2% on placebo. No one died in those trials, but the pattern was strong enough to demand action.
Who Does the Warning Apply To?
The warning covers all antidepressants, including SSRIs like fluoxetine (Prozac), sertraline (Zoloft), escitalopram (Lexapro), and others like venlafaxine (Effexor) and bupropion (Wellbutrin). In 2006, the FDA expanded it to include young adults up to age 24, not just teens.There are exceptions. Fluoxetine is still approved for treating depression in children as young as 8. Sertraline and fluvoxamine are approved for OCD in kids. These drugs were studied more closely and showed a better risk-benefit balance in younger populations. But for most other antidepressants, the warning applies across the board.
It’s important to know: the warning doesn’t say you shouldn’t take these meds. It says: be aware, monitor closely, and don’t stop without talking to your doctor.
Why Does This Happen?
It’s not fully understood why some people experience this surge in suicidal thinking early on. But experts have a few theories.One idea is that antidepressants can restore energy before they lift mood. Someone who’s been too exhausted to act on suicidal thoughts might suddenly have the physical ability to do so-even if they still feel hopeless. Another theory is that as brain chemistry begins to shift, anxiety or agitation can spike temporarily, making emotional pain feel more overwhelming.
This usually happens in the first two to four weeks. After that, for most people, the risk goes down. That’s why the first month of treatment is the most critical. It’s not the drug itself causing suicide. It’s the transition phase-when the body is adjusting, and the person is still in deep emotional pain.
The Unintended Consequences
Here’s where things get complicated. After the black box warning went into effect, prescriptions for antidepressants in young people dropped by more than 22%. Psychotherapy visits fell too. And guess what happened next?In the years that followed, suicide rates among teens and young adults in the U.S. rose. A 2023 study in Health Affairs found that after the warning, youth suicide deaths increased by nearly 15%. Emergency room visits for drug poisonings-often self-harm attempts-went up by 29%.
Why? Because some families, scared by the warning, avoided treatment entirely. Others stopped medication too soon. Some doctors became hesitant to prescribe. And without treatment, depression doesn’t get better on its own. In fact, untreated depression carries a much higher risk of suicide than any medication.
One study followed two teens with major depression who refused antidepressants after learning about the black box warning. Both later attempted suicide. Their families believed they were protecting them by avoiding medication-but the untreated illness was the real danger.
What Do Experts Really Think?
There’s a fierce debate among researchers. The FDA stands by its warning, citing controlled trial data showing increased suicidality. Some psychiatrists agree, pointing to case-control studies that show higher suicide attempts among youth taking antidepressants-even after adjusting for severity of illness.But others argue the warning has done more harm than good. A 2020 paper in PMC criticized studies claiming the warning caused harm, calling them methodologically weak. Yet another 2023 analysis, using more robust real-world data, found the opposite: the warning led to fewer treatments, more self-harm, and more deaths.
Even the American Psychiatric Association says this: the benefits of antidepressants for most young people with moderate to severe depression outweigh the risks. They stress that the warning should not scare people away from treatment-it should guide safer monitoring.

What Should You Do?
If you or someone you love is starting an antidepressant, here’s what matters most:- Don’t panic. The risk is real, but small-and temporary.
- Watch closely during the first month. Look for new or worsening symptoms: talking about death, giving away belongings, withdrawing, acting recklessly, or sudden mood swings.
- Keep all follow-up appointments. The first check-in should be within one to two weeks. Don’t skip it.
- Don’t stop the medication suddenly. Stopping can cause withdrawal symptoms and make depression worse.
- Call your doctor immediately if you notice any signs of increased suicidal thinking.
- Involve a trusted person. Have someone check in daily during the first few weeks. Isolation is dangerous.
For parents: Talk to your teen about this warning before they start. Say something like: "This medicine might make you feel more restless or upset at first. That doesn’t mean it’s not working. But if you ever feel like you want to hurt yourself, tell me right away. We’ll get help."
Is There a Better Way?
Many experts now agree: the one-size-fits-all black box warning is outdated. Not all antidepressants carry the same risk. Paroxetine, for example, has shown higher rates of suicidality in studies. Fluoxetine has shown the lowest. A 2021 meta-analysis in JAMA Psychiatry found that risk varies significantly by drug.Instead of one warning for all antidepressants, experts recommend:
- Medication-specific warnings
- Clearer language that distinguishes between "increased risk" and "causes suicide"
- Stronger emphasis on monitoring, not avoidance
- Guidance for doctors to choose antidepressants with lower risk profiles for younger patients
The FDA reviewed new evidence in 2022 and kept the warning-but added slight tweaks to the wording to better explain the risk-benefit balance. That’s a step forward. But the real change needs to come from how we talk about it.
Bottom Line
Antidepressants aren’t magic pills. They’re tools. And like any tool, they work best when used with care. The black box warning exists not to scare you away from treatment-but to make sure you get the right support at the most vulnerable time.If you’re depressed, you’re not alone. If you’re scared to start medication, that’s normal. But don’t let fear keep you from getting help. Untreated depression is far more dangerous than the risk of a temporary increase in suicidal thoughts.
With proper monitoring, most people who start antidepressants don’t experience this side effect. And for those who do, early detection saves lives.
Do antidepressants cause suicide?
No, antidepressants do not cause suicide. But in a small number of children, adolescents, and young adults under 24, they may increase the risk of suicidal thoughts or behaviors during the first few weeks of treatment. This is not the same as causing suicide-it’s a temporary surge in risk that usually fades as the medication starts working. The bigger danger is leaving depression untreated.
Which antidepressants have the highest risk of suicidal thoughts?
Studies suggest paroxetine carries a higher risk compared to others. Fluoxetine (Prozac) has shown the lowest risk in young people and is often recommended as a first choice for teens. Sertraline and fluvoxamine also have favorable safety profiles for pediatric use. But individual responses vary, so your doctor should pick the best option based on your history and symptoms.
What should I do if I start feeling worse on antidepressants?
If you notice new or worsening suicidal thoughts, agitation, panic attacks, or extreme restlessness, contact your doctor immediately. Don’t wait for your next appointment. Call your prescriber, go to an emergency room, or call a crisis line. These symptoms often appear in the first two weeks and can be managed if caught early. Stopping the medication without guidance can make things worse.
Can I still take antidepressants if I’ve had suicidal thoughts before?
Yes, many people with a history of suicidal thoughts benefit from antidepressants. The key is close monitoring. Your doctor may choose a lower-risk medication like fluoxetine, start with a lower dose, schedule more frequent check-ins, and pair treatment with therapy. The goal is not to avoid medication-it’s to manage the risk safely.
Is it safe to stop antidepressants if I’m worried about the warning?
No. Stopping abruptly can cause withdrawal symptoms, rebound depression, and increased suicide risk. If you’re concerned, talk to your doctor. They can help you adjust your treatment plan safely. Never stop medication without medical supervision-even if you’ve heard scary stories about the black box warning.
Are there alternatives to antidepressants for teens and young adults?
Yes. Cognitive behavioral therapy (CBT) and interpersonal therapy (IPT) are proven to help depression in young people, especially for mild to moderate cases. For severe depression, combining therapy with medication often works best. Lifestyle changes-like regular sleep, exercise, and reducing screen time-help too. But for many, medication is necessary. The choice isn’t either/or-it’s what works best for you.

Gillian Watson
Been on sertraline for 3 years now. The first month was rough but I didn’t have suicidal thoughts, just felt like a robot. My doctor warned me about the black box but honestly, the silence after starting meds was worse than any side effect. Now I’m functional. Just need patience and someone to check in.
Jordan Wall
Let’s be real-this whole black box narrative is a classic case of regulatory overreach masquerading as harm reduction. The FDA’s data is cherry-picked from underpowered RCTs with no real-world confounder adjustment. You’re telling me a 1.8% absolute risk increase in suicidality (mostly ideation, not attempts) justifies a 22% drop in Rx rates? That’s not caution, that’s panic-driven public health malpractice. 🤦♂️
Shofner Lehto
As a therapist who’s worked with teens for 15 years, I’ve seen this play out too many times. The warning wasn’t meant to scare people off-it was meant to create space for dialogue. The real tragedy isn’t the medication, it’s the silence that follows when families hear ‘black box’ and assume ‘deadly’. We need better education, not fear.
Elizabeth Crutchfield
i had the same thing happen with lexapro… i felt like i was gonna jump out my skin for like 2 weeks. i thought i was gonna kill myself but it was just anxiety on steroids. my mom stayed home with me and we watched dumb netflix till it passed. now i’m good. dont stop.
Ben Choy
Just want to say this post saved my life. I was about to quit my meds after reading a scary Reddit thread. But then I saw the stats about suicide rates going up after prescriptions dropped. I talked to my doctor and we switched to fluoxetine. 4 months in and I’m actually smiling again. 💙
Emmanuel Peter
Let me get this straight-you’re telling me we should give SSRIs to 14-year-olds who just got dumped on TikTok? This isn’t medicine, it’s chemical pacification. The real problem is social decay, not serotonin. Give them a hobby, a mentor, a damn purpose instead of a pill. You’re medicating the symptom, not the cause.
Ashley Elliott
Important note: The black box warning applies to ‘suicidal ideation’-not suicide attempts or completion. That distinction matters. Also, the risk peaks at 2–4 weeks and drops off sharply after 8. Monitoring isn’t optional-it’s the difference between life and a preventable tragedy. Please, if you’re reading this and you’re scared-call your provider. You’re not alone.
Scott van Haastrecht
So let me get this straight. You’re saying the drug companies didn’t manipulate the data? The FDA didn’t bow to pharma pressure? And the fact that 15% more teens died after this warning is just a coincidence? Wake up. This is corporate medicine at its finest. They profit from lifelong prescriptions, not recovery.
Chase Brittingham
I’m 21 and I started on fluoxetine last year. I had zero suicidal thoughts but I did get really jittery for a week. My therapist had me text her every night. That’s what made the difference-not the warning, not the drug, but the human connection. If you’re scared, find someone who’ll sit with you. You don’t have to do this alone.
Bill Wolfe
It’s not just about the black box-it’s about the cultural collapse that led us to medicate existential despair. We’ve turned emotional suffering into a diagnostic category, then outsourced healing to pharmacology. The real issue isn’t SSRIs-it’s a society that’s forgotten how to hold space for pain. And now we’ve got a generation of kids on pills because no one taught them how to cry without a prescription.
Ollie Newland
As a GP, I’ve prescribed over 300 antidepressants to under-25s. The black box is a necessary safeguard, but it’s useless without follow-up. The real failure? Patients getting the script and never seeing a provider again. If you’re on one, get scheduled for week 2. If you’re a parent, ask your kid if they’ve had any dark thoughts-not in a scary way, just like, ‘Hey, how’s your head feeling?’