Why Your Family Needs an Overdose Emergency Plan
Every year, over 100,000 people in the U.S. die from drug overdoses. Most of these deaths involve prescription opioids or synthetic drugs like fentanyl. And here’s the hard truth: overdose deaths often happen at home, with family members present but unprepared. If someone in your household takes opioids for chronic pain, or even just keeps them as a backup, you’re not immune. You might think, "It won’t happen to us." But 63% of preventable overdose deaths happen because people wait too long to act. That’s why a simple, written plan can save a life.
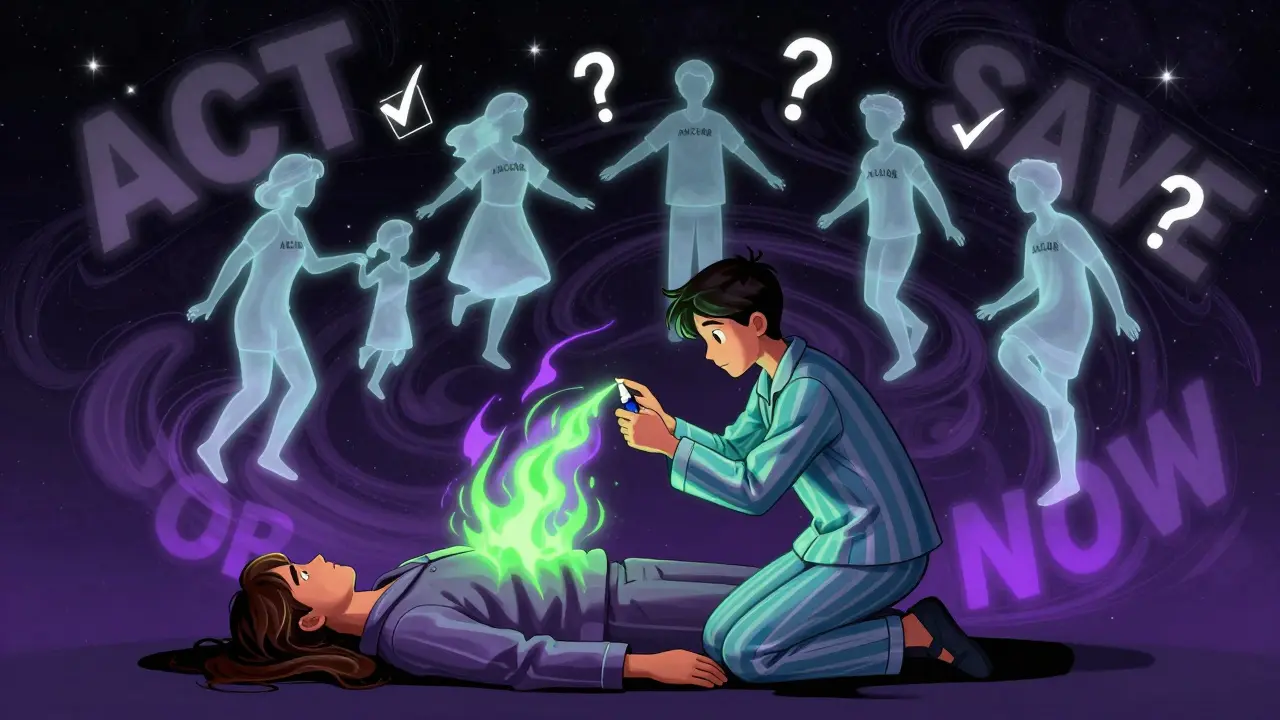
An overdose emergency plan isn’t about fear. It’s about readiness. Think of it like a fire extinguisher in the kitchen. You hope you never need it. But if you do, you want it right there, you know how to use it, and everyone else in the house does too. Naloxone - the medication that reverses opioid overdoses - works in under five minutes. But only if someone grabs it and uses it fast. Without a plan, people freeze. They panic. They call 911 first, wasting precious minutes. With a plan, they act.
Step 1: Know Who’s at Risk
Not every family needs this plan. But if someone in your home takes opioids - even just one prescription - you should make one. Opioids include medications like oxycodone, hydrocodone, morphine, and fentanyl patches. The CDC says over 51 million U.S. adults got opioid prescriptions in 2022. That’s one in five households. Risk goes up if someone:
- Takes more than 50 morphine milligram equivalents (MME) per day
- Uses opioids with alcohol, benzodiazepines (like Xanax), or sleep meds
- Has a history of substance use disorder
- Has breathing problems like sleep apnea
- Has recently been released from jail or a hospital after stopping use
Don’t assume risk only comes from illegal drugs. Most overdose deaths involve legally prescribed medications. If you’re unsure, check the bottle. If it says "opioid" or has a black box warning, you need a plan.
Step 2: Get Naloxone - Now
Naloxone is the only medication that can reverse an opioid overdose. It’s safe, non-addictive, and works even if the person took fentanyl. In 2023, the FDA approved generic versions, making it cheaper than ever. You can get it without a prescription at most pharmacies in 46 states. CVS, Walgreens, and many independent pharmacies keep it behind the counter - just ask.
Buy two or three doses. Fentanyl is so strong that one dose of naloxone often isn’t enough. The Washington State Health Department recommends keeping at least two kits on hand. Each kit includes:
- One or two nasal sprays (Narcan or generic)
- Instructions
- Disposable gloves (sometimes)
Cost? Around $25-$40 without insurance. With Medicare Part D or most private plans, it’s now $0 copay thanks to the 2024 Inflation Reduction Act. If you’re still being charged, ask for a different brand or call your insurer. You can also get free kits from local health departments, harm reduction centers, or community programs - especially in cities like Melbourne, where public health outreach is strong.
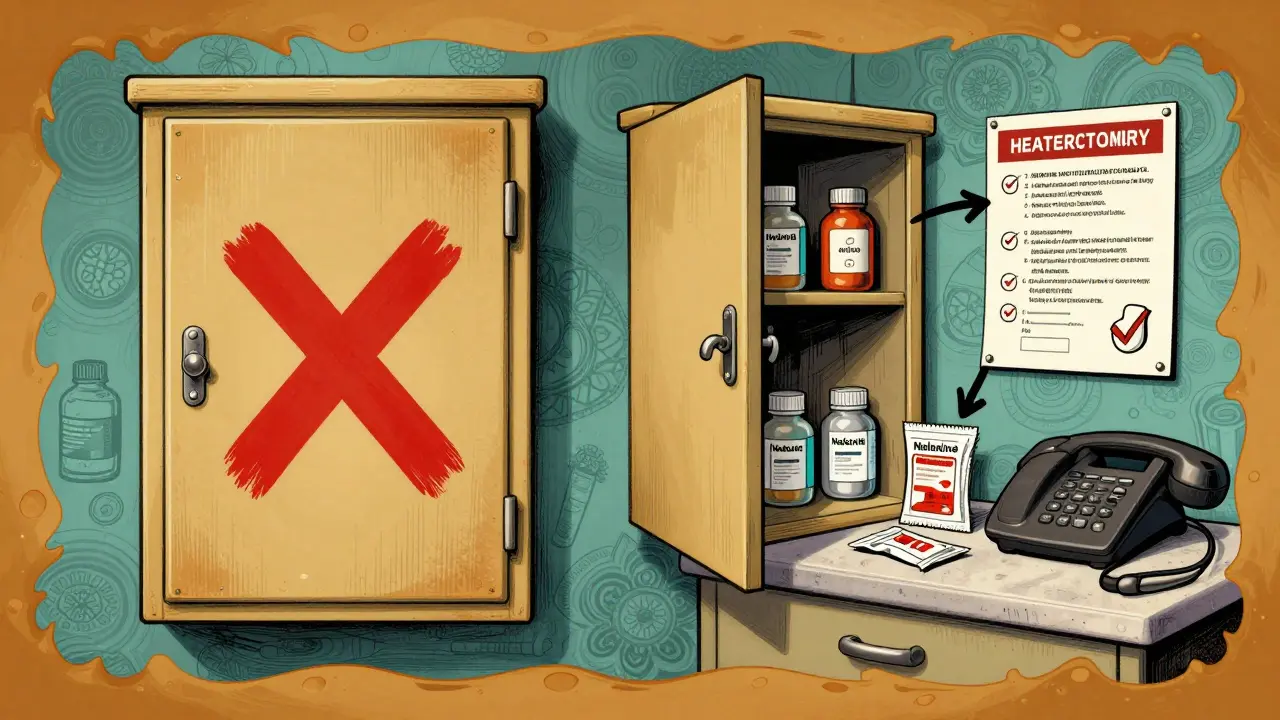
Step 3: Store It Right - And Make It Accessible
Storing naloxone in a locked cabinet defeats the whole purpose. It needs to be:
- At room temperature (68-77°F)
- Out of direct sunlight
- Easy for anyone to find - not hidden in a drawer
Put it near your phone, your first aid kit, or your front door. Something everyone sees daily. Don’t store it in the bathroom - heat and moisture ruin it. Don’t keep it in the car - summer heat can make it useless. Check the expiration date every 18 months. Naloxone doesn’t expire instantly, but its effectiveness drops after two years. Replace it before then.
Step 4: Learn the Signs of Overdose
An overdose doesn’t always look like a movie. People don’t always collapse. They might just be very still. Look for these three signs:
- Unresponsive - Shake their shoulder, shout their name. If they don’t wake up, it’s not sleep. It’s overdose.
- Slow or no breathing - Count breaths for 15 seconds. If they take fewer than four breaths, they’re in danger. Lips or fingernails turning blue is a late sign.
- Pinpoint pupils - Shine a light in their eye. If the black center is tiny like a pinprick, it’s a classic opioid sign.
Don’t wait for all three. If two are present, act. Fentanyl can knock someone out in under three minutes. Waiting for the third sign could be fatal.
Step 5: Practice the Response - Every Time
There’s a big gap between knowing what to do and doing it under stress. That’s why you need to practice. Use the A.N.C.H.O.R. method:
- Assess - Check for responsiveness and breathing.
- Naloxone - Spray one dose into one nostril. No need to tilt the head. Just insert and push the plunger.
- Call 911 - Do this right after giving naloxone. Say: "Someone has overdosed on opioids. I’ve given naloxone. They’re not breathing." Don’t wait to see if it works.
- Have more ready - Keep the second dose nearby. If they don’t wake up in 3-5 minutes, give another.
- Observe - Stay with them. Even if they wake up, they can relapse into overdose in the next 2-4 hours. Keep them awake and talking. Don’t let them go back to sleep.
- Review - After it’s over, talk as a family. What worked? What confused you? Update the plan.
Practice this sequence once a month. Just 10 minutes. Use a toy or a pillow to simulate the person. Get your kids involved. Teens are often the first to find someone unresponsive. They need to know what to do too.
Step 6: Write It Down - And Keep It Visible
Write your plan on a small card. Laminate it. Put it on the fridge, next to the phone, or in your wallet. Include:
- Names and doses of all opioids in the home
- Names and phone numbers of prescribing doctors
- Location of naloxone kits
- Emergency contacts (including poison control: 1-800-222-1222)
- Step-by-step instructions in simple language
Ohio’s 2022 trial showed this reduces response time by nearly 50 seconds. In an emergency, every second counts. A written plan also helps EMS when they arrive. They’ll ask: "Did you give naloxone? What did they take?" You’ll have the answers.
What This Plan Won’t Do
It won’t fix addiction. It won’t stop someone from using. But it will give them a chance to get help. Studies show 89% of people who survive an overdose with naloxone go on to seek treatment. That’s not a coincidence. Surviving changes everything.
This plan also won’t help with overdoses from alcohol, benzodiazepines, or stimulants like cocaine or meth. Those require different responses - mostly calling 911 and keeping the person safe until help arrives. But for opioids? This plan is your best tool.
Real Stories, Real Results
One mother in Ohio used her Narcan kit on her 22-year-old son after finding him blue and not breathing. "I sprayed it in both nostrils. Three minutes later, he coughed. Ten minutes later, he was talking. EMS came 12 minutes after that. He’s alive because we had the plan. We practiced. We didn’t wait."
Another family in Oregon kept their naloxone in the glovebox. When their daughter overdosed, they couldn’t find it. She didn’t survive. Her brother now carries two kits in his backpack.
These aren’t rare. They’re common. And they’re preventable.
What to Do After an Overdose
Even if naloxone works, the person still needs medical care. Naloxone wears off in 30-90 minutes. Opioids stay in the body much longer. That’s why people can die hours later - it’s called "renarcotization." Stay with them. Don’t let them go to sleep. Call 911 even if they seem fine. Tell the paramedics what you gave and when.
Afterward, talk to your family. Was it traumatic? Was it confusing? Did you wish you’d known more? Use that experience to update your plan. Make it better. Share it with others. One plan can save more than one life.
Where to Get Help
You don’t have to do this alone. Free training is available:
- American Red Cross - 15-minute online course (free)
- Washington State OEND - In-person training at local clinics
- NYC Project COPE - Free kits + training for families
- Local health departments - Most offer free naloxone and instruction
Check your city or state health website. In Australia, similar programs exist through state health services. If you’re in Melbourne, contact the Victorian Department of Health for local resources.
Final Thought: Be the Person Who Acts
Most people who die from overdose are found by family. That means you’re the first responder. You don’t need medical training. You just need to know what to do - and do it without hesitation. A plan turns panic into action. It turns fear into power. And in a moment when seconds matter, that’s everything.
Can I get naloxone without a prescription?
Yes. In 46 U.S. states, you can buy naloxone directly at pharmacies without a prescription. In Australia, naloxone is available over the counter at pharmacies under the Pharmacy Only (Schedule 3) classification. You can ask the pharmacist for it - no questions asked.
Is naloxone safe to use if I’m not sure it’s an opioid overdose?
Yes. Naloxone has no effect on people who haven’t taken opioids. If someone is unresponsive and you suspect an overdose, give it anyway. It won’t harm them. The worst-case scenario is you waste a dose. The best-case is you save a life.
What if the person wakes up after I give naloxone? Do I still need to call 911?
Yes. Even if they seem fine, naloxone wears off faster than the opioid. They can slip back into overdose within 30 to 90 minutes. Medical professionals need to monitor them for at least 2-4 hours. Never assume they’re out of danger.
How often should I replace my naloxone kit?
Check the expiration date on the box. Most kits last 18-24 months. Replace them before they expire. Even if the spray looks fine, the medication can lose potency. Don’t wait until it’s too late.
Can children or teens use naloxone?
Yes. Naloxone nasal spray is simple to use - no needles, no training needed. Teens as young as 12 have successfully used it in emergencies. Train them just like you would teach them to use a fire extinguisher. Practice with them. Confidence saves lives.
Will I get in trouble if I call 911 during an overdose?
No. All 50 U.S. states have Good Samaritan laws that protect people who call for help during an overdose. You won’t be arrested for drug possession if you’re reporting an emergency. In Australia, similar protections exist under state health legislation. Calling 911 is the right thing to do - and legally protected.
What if I don’t have insurance? Can I still afford naloxone?
Yes. Generic naloxone nasal spray costs as little as $25 at many pharmacies. Many community health centers and harm reduction programs give it away for free. In Melbourne, contact local pharmacies or the Victorian Alcohol and Drug Information Service for free kits. You don’t need insurance to save a life.
Next Steps: Start Today
Don’t wait for a crisis to act. Pick up a naloxone kit this week. Talk to your family. Practice the steps. Write down your plan. Put it on the fridge. You’re not being dramatic. You’re being smart. And you’re giving your family the best chance to survive - because sometimes, the only thing between life and death is a spray bottle and someone who knows how to use it.

Sam Davies
Oh wow, a *family overdose emergency plan*? How quaint. Next you’ll be suggesting we all keep a fire extinguisher next to our Netflix remote. At least this one doesn’t require a subscription. I mean, really-Naloxone? On the fridge? Like a grocery list? I’m sure the opioid crisis is just waiting for someone to misplace it between the ketchup and the expired coupons.
Jennifer Littler
This is clinically sound and aligns with CDC harm reduction protocols. Key elements: accessibility of naloxone, multi-dose redundancy, and structured A.N.C.H.O.R. protocol reduce mortality by up to 68% in peer-reviewed studies (JAMA, 2023). Implementation requires standardized education modules-ideally integrated into primary care workflows. Consider embedding this into EHR alerts for high-risk prescriptions.
Alfred Schmidt
I’ve seen this crap before. People think a spray bottle is a magic bullet. NO. It’s not. You don’t just ‘spray and pray.’ You need to know the difference between opioid overdose and diabetic coma. You need to know if they’re on benzodiazepines too. And you think your kid’s gonna remember the steps after watching a TikTok? Please. This plan is a feel-good illusion. Real help requires rehab, not a laminated card stuck to the fridge with a magnet shaped like a heart.
Priscilla Kraft
This is so important 💗 I just got my first naloxone kit last week after my cousin’s near-miss. I put it next to the coffee maker so everyone sees it daily 😊 I taught my 14-year-old how to use it-she practiced on a pillow and even made flashcards! We did a family drill last Sunday 🙌 I know it sounds dramatic but honestly? It feels like giving your family superpowers. If you’re reading this and haven’t gotten one yet… please just do it. You won’t regret it. Ever. 🙏
Michael Patterson
Okay so first off this whole thing is a bit of a scare tactic. Yeah 100k overdoses a year but like… most of those are people who are actively using and don’t have families who care. And yeah naloxone is great but it’s not a cure. It’s a bandaid on a bullet wound. And you say don’t store it in the bathroom but what if you live in a 500 sq ft apartment? You gonna put it on the toaster? Also I’ve seen people give naloxone and then just leave. Like what? You think they’re fine? Nah. They’re gonna crash again. And the whole ‘practice every month’ thing? Sounds like a cult. Also typo: ‘fentany’ in step 2. Fix that.
Matthew Miller
This is performative activism dressed as public health. You’re not saving lives-you’re creating a false sense of security. People who overdose are not victims of bad planning. They’re victims of poor choices, weak wills, and systemic failure. Handing out naloxone like candy is just enabling. If someone’s using opioids recreationally, they shouldn’t be in your home. And if they’re prescribed them? Then their doctor should be managing the risk-not you. This plan is a distraction from the real problem: addiction is a moral failure disguised as a medical condition.
Roshan Joy
This is very thoughtful. I live in India and we don’t have easy access to naloxone here, but I shared this with my cousin who works in a hospital in Delhi. She said they’re starting to train nurses in basic overdose response-no naloxone yet, but at least they know to check breathing and call for help. Maybe one day. Thank you for writing this clearly. I printed it out and gave it to my sister who takes pain meds after her surgery. She said she felt less scared now.
Adewumi Gbotemi
I like this. Simple. No fancy words. My cousin in Lagos had a bad reaction to painkillers last year. No one knew what to do. He lived, but just barely. I’m getting two kits next week. I’m putting one in my bag and one at home. My kids are 7 and 9. I’ll teach them how to press the spray. No need for big talk. Just do it.
Priya Patel
I just cried reading this. My brother OD’d two years ago. We didn’t have naloxone. We panicked. We called 911… then waited. He made it. But he’s not the same. I wish I’d known then what I know now. I keep my kit in the drawer next to the TV remote. We all know where it is. We practiced last weekend. My mom cried. My dad laughed nervously. But we did it. And I’m telling everyone I know. This isn’t fear. It’s love. 💕
Jason Shriner
So we’re just supposed to… spray someone in the nose and call it a day? Like, what’s next? A QR code on the fridge that links to a YouTube tutorial? This feels like a corporate wellness pamphlet written by someone who’s never held a dying person. Naloxone isn’t a magic wand. It’s a temporary reset button. And the real tragedy? Most people who survive this… end up back where they started. So what’s the point? We’re just delaying the inevitable with a $40 spray.
Sean Feng
Naloxone works