Anemia: Understanding the Basics and How to Manage It
When dealing with Anemia, a condition marked by low red blood cell count or reduced hemoglobin. Also known as low blood count, it often shows up as fatigue, shortness of breath, or pale skin. Iron deficiency is one of the most common triggers, while Vitamin B12 shortage can produce similar signs. The level of Hemoglobin is the key lab marker doctors watch. In some cases, especially kidney disease, Erythropoietin therapy becomes essential. These pieces fit together to define what anemia really means for you.
Anemia encompasses a wide range of blood‑related problems, so figuring out the exact cause matters. Iron deficiency lowers the body’s ability to make hemoglobin, which in turn reduces oxygen delivery to tissues. Vitamin B12 deficiency, on the other hand, disrupts DNA synthesis in red‑cell precursors, leading to larger but fewer cells – a condition called megaloblastic anemia. Both scenarios show how nutrient gaps directly influence hemoglobin production, creating a clear cause‑effect chain. Understanding this chain helps you choose the right supplement or medication, rather than guessing.
Common Causes and Treatments
Most people think anemia is just about iron, but chronic disease, blood loss, and genetic traits also play a role. Chronic kidney disease reduces natural erythropoietin output, so doctors may prescribe synthetic erythropoietin to boost red‑cell creation. Heavy menstrual periods or gastrointestinal bleeding can silently drain iron stores, requiring iron pills or dietary changes. For those with B12 shortage, oral tablets or injectable forms are the go‑to solutions. Each treatment targets a specific underlying factor, showing why a personalized plan beats a one‑size‑fits‑all approach.
Diet matters, too. Red meat, beans, and leafy greens give you iron that the body can absorb, especially when paired with vitamin C. Vitamin B12 lives in animal products, so vegans often need fortified foods or supplements. Knowing which foods affect which deficiency helps you fine‑tune your meals without relying solely on pills. When diet alone isn’t enough, physicians can add prescription‑strength iron or B12, and they’ll monitor hemoglobin levels regularly to see if the therapy is working.
Testing is a simple but powerful tool. A complete blood count (CBC) tells you hemoglobin and hematocrit values, while ferritin and transferrin saturation gauge iron stores. If B12 is low, a serum B12 test or methylmalonic acid level will point the finger at a deficiency. In complex cases, a bone‑marrow biopsy might be ordered, but that’s rare. The goal is to pinpoint the exact reason for low red‑cell numbers, because treating the wrong cause won’t raise your energy levels.
When you’ve identified the culprit, managing side effects becomes the next step. Iron supplements can cause constipation or stomach upset, so taking them with food—or switching to a lower‑dose, slow‑release formula—can help. Vitamin B12 injections are usually painless, but some people feel a slight sting. If you’re on erythropoietin, doctors will watch your blood pressure, as the medication can raise it in a small number of patients. Being aware of these nuances lets you stay ahead of problems.
Beyond medication, lifestyle tweaks support recovery. Regular light exercise boosts circulation and helps the body use oxygen more efficiently, which can lessen fatigue even before hemoglobin fully rebounds. Adequate sleep, stress reduction, and staying hydrated all play a part in overall blood health. Think of it as a team effort: supplements, diet, meds, and healthy habits each have a role in restoring your blood’s oxygen‑carrying capacity.
Sometimes anemia is a sign of something bigger, like an autoimmune disorder or a hidden infection. If standard iron or B12 therapy doesn’t lift your numbers, doctors may dig deeper, looking for conditions like lupus, rheumatoid arthritis, or inflammatory bowel disease. These illnesses can interfere with nutrient absorption or directly destroy red cells. Recognizing anemia as a potential red flag encourages early detection of serious health issues.
Finally, keep track of your progress. Most people see a rise in hemoglobin within a few weeks of starting the right treatment, but full recovery can take months. Use a simple log to note energy levels, exercise tolerance, and any side effects. Share this information with your healthcare provider so they can adjust doses or switch therapies if needed. The more data you collect, the faster you’ll get back to feeling like yourself.
With this background, you’ll find the articles below much easier to navigate. They dive into specific drugs, supplements, and strategies that target the various forms of anemia we’ve just discussed, giving you practical steps you can take right now. Explore the collection to see how each option fits into the bigger picture of blood health.
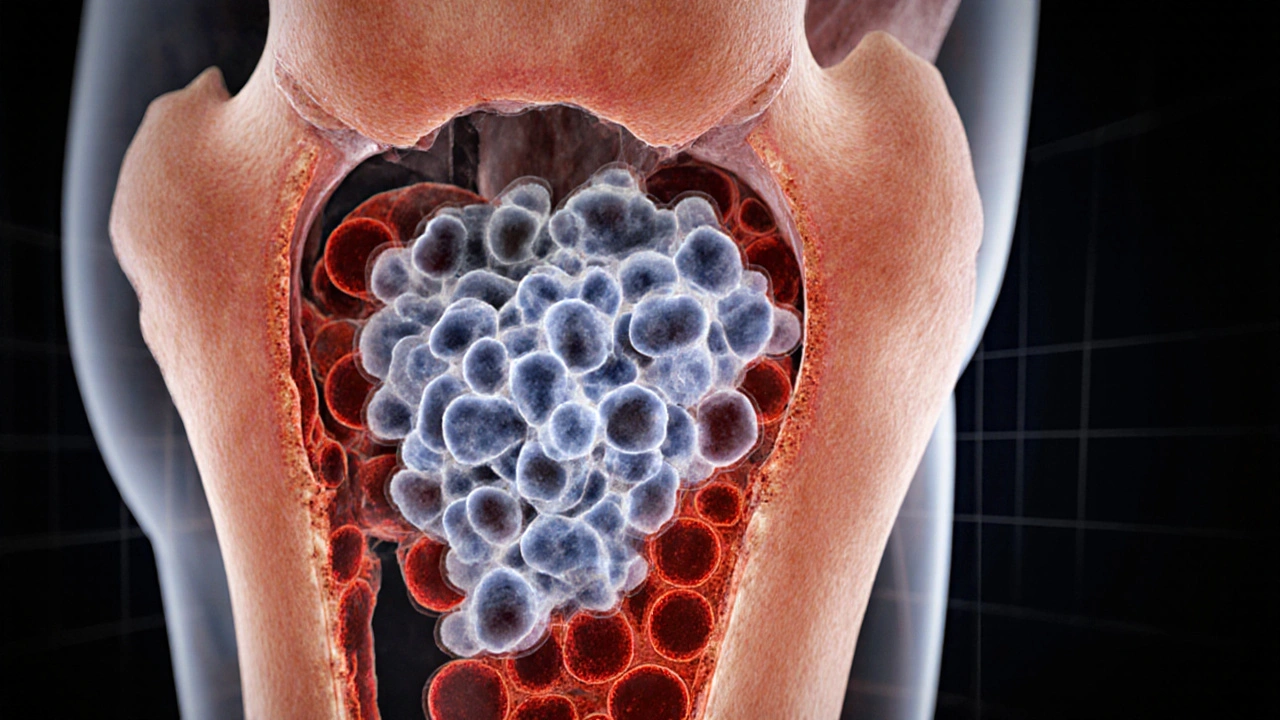
Leukemia and Anemia: Key Connections You Must Know
Learn how leukemia leads to anemia, recognize overlapping symptoms, understand diagnostic tests, and discover effective management strategies for both conditions.