Every year, millions of older adults take more medications than they need. Some of these drugs were prescribed years ago for conditions that have changed-or disappeared. Others were meant to prevent future problems, but now the risks outweigh the benefits. This isn’t laziness or oversight. It’s the natural result of how medicine works: we add drugs, rarely remove them. But a quiet revolution is happening in clinical practice-deprescribing. It’s not about cutting corners. It’s about thinking smarter.
What Exactly Is Deprescribing?
Deprescribing isn’t just stopping pills. It’s a careful, step-by-step process where doctors and patients work together to decide which medications can be safely reduced or stopped. The goal? To reduce harm, improve quality of life, and stop treating past problems with today’s drugs. According to the American Geriatrics Society, deprescribing means “the planned and supervised process of dose reduction or stopping of medication that might be causing harm, or no longer be of benefit.” It’s the mirror image of prescribing. Just as you wouldn’t start a new drug without checking for interactions, side effects, and patient goals, you shouldn’t keep one without the same scrutiny. This isn’t theoretical. In Australia, about 30% of people over 65 take five or more medications daily. In the U.S., that number hits 40%. And 20% of older adults are on ten or more. That’s not just polypharmacy-it’s a systemic issue. And research shows it’s linked to falls, confusion, kidney stress, and hospital visits.The Five Steps of Safe Deprescribing
Deprescribing follows a clear structure. It’s not guesswork. Here’s how it works in real practice:- Identify potentially inappropriate medications. This means looking at each drug on the list. Is it still needed? Is it a preventive drug (like a statin or aspirin) for someone with advanced dementia or a life expectancy under two years? If yes, it’s a candidate.
- Determine if it can be reduced or stopped. Not all drugs can be cut cold turkey. Some, like benzodiazepines or antidepressants, need slow tapering to avoid withdrawal. Others, like antacids or blood pressure meds, can often be stopped with minimal risk.
- Plan the taper. This isn’t one-size-fits-all. A patient with mild kidney issues might stop a diuretic over two weeks. Someone on long-term opioids might need months. The plan includes how fast to reduce, what symptoms to watch for, and when to check back in.
- Monitor for changes. After stopping, patients are watched closely. Do they feel better? Worse? Do symptoms return? Sometimes, stopping a drug leads to improved energy or sleep. Other times, a symptom comes back-but now you know if it was drug-induced or disease-related.
- Document everything. What was stopped? When? Why? What happened? This isn’t bureaucracy. It’s critical for future care. If a patient sees a new doctor, they need to know this wasn’t an accident-it was intentional.
What Does the Research Say About Outcomes?
The biggest question: Does deprescribing actually help people live better-or just save money? A 2023 review in JAMA Network Open looked at 67 studies involving over 20,000 older adults. The results were clear: deprescribing reduced the average number of medications per person by about one. Sounds small? It’s not. Think of it this way: a doctor with 2,000 patients, half of whom are on five or more drugs, could safely reduce over 140 medications in a year. That’s 140 fewer chances for a bad reaction, fewer drug interactions, less confusion, fewer falls. But here’s the catch: most studies didn’t measure long-term outcomes like death, hospitalization, or mobility. They measured pill counts. That’s why some critics say the evidence is weak. A 2013 Canadian study found no significant drop in hospital visits or deaths after deprescribing. But they admitted the studies were too short and too small to catch real benefits. Newer research is changing that. A 2024 study in the Journal of the American Geriatrics Society found that when deprescribing was done properly-with follow-ups and patient input-people reported better sleep, less dizziness, and improved mental clarity. Falls dropped by 18% in one trial. In another, patients on proton pump inhibitors (PPIs) for heartburn who stopped them had no increase in reflux symptoms, but did report less bloating and gas. The Agency for Healthcare Research and Quality (AHRQ) now lists deprescribing as proven to reduce morbidity, improve mental status, and cut hospital admissions. The evidence isn’t perfect-but it’s growing fast.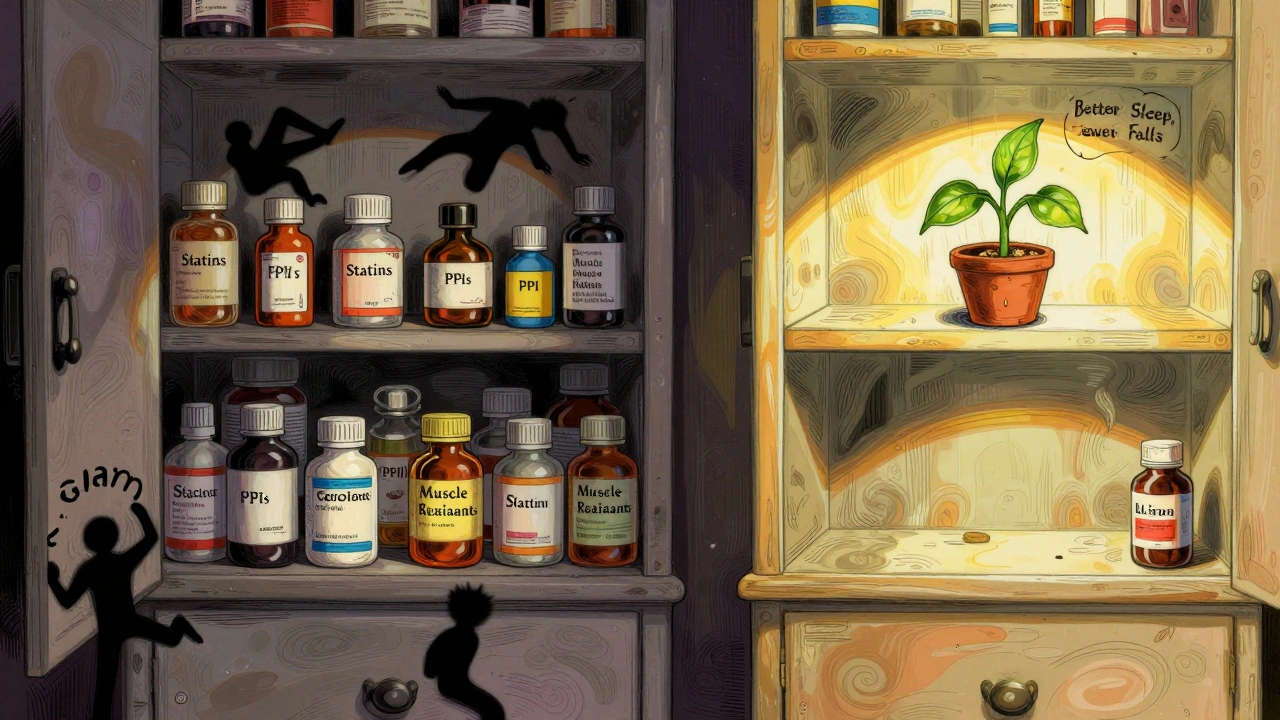
Why Don’t More Doctors Do It?
If it’s so good, why isn’t it routine? One reason: fear. Doctors worry about backlash. “What if I stop this and they get worse?” “What if they sue?” Another: time. Reviewing a patient’s entire med list takes 15-20 minutes. Most appointments are 10. And then there’s the patient side. Many older adults believe if a doctor gave them a pill, it must be necessary. They don’t question it. A 2019 study from the American Academy of Family Physicians found that patients want to take fewer meds-but almost never bring it up themselves. They wait for the doctor to start the conversation. That’s why the most successful deprescribing programs don’t just tell doctors to stop drugs. They train them to ask: “Is this still helping you?” “What are your goals right now?” “Would you be okay trying to go without this one?”Real-Life Scenarios: What Works
Take Mrs. Chen, 82, living alone in Melbourne. She’s on 11 medications: blood pressure pills, a statin, a daily aspirin, a PPI for acid reflux, a sleep aid, a muscle relaxant, and more. She’s had two falls in the past year. Her memory is fading. Her daughter says she’s always sleepy. Her GP didn’t just cut pills. They sat down. Asked: “What matters most to you right now?” Mrs. Chen said: “I want to walk without falling. I want to feel awake during the day.” They stopped the sleep aid first. Then the muscle relaxant. Then the aspirin-her heart risk was low, and bleeding risk was rising. Three months later, she hadn’t fallen again. Her energy improved. Her PPI was reduced by half. She still takes her blood pressure meds-those are still helping. Or Mr. Rivera, 78, with advanced heart failure and dementia. He was on a long list of preventive drugs: a cholesterol pill, a diabetes med, a bone density drug. None of these were helping him live better. He couldn’t remember to take them. His family was stressed. His doctor stopped them all. Within weeks, his caregiver said he seemed calmer. Less confused. No side effects. No rebound issues. These aren’t outliers. They’re becoming common in clinics that use structured deprescribing tools.
What’s Next? The Future of Deprescribing
The next big push is integration. Right now, deprescribing is done in pockets-by passionate GPs, pharmacists, or geriatric teams. But the future is in electronic health records. The American Academy of Family Physicians is testing a new tool that flags high-risk meds during patient visits. In pilot clinics, it led to a 15% drop in inappropriate prescriptions. That’s huge. Researchers are also building algorithms that predict which drugs are safest to stop based on age, kidney function, and genetic markers. Early work shows people with certain gene variants metabolize benzodiazepines slower-meaning they’re at higher risk for falls. That’s personalized deprescribing. And patient resources are growing. The website deprescribing.org has been downloaded over half a million times. It offers printable checklists, conversation starters, and even scripts for families to use with doctors. The big picture? As the population ages, polypharmacy will only get worse. By 2030, one in five Americans will be over 65. In Australia, it’s already one in five. Without action, more people will end up in hospitals from drug reactions than from falls or infections. Deprescribing isn’t a trend. It’s a necessary shift in how we think about medicine. It’s not about doing less. It’s about doing better.What Patients Can Do Today
You don’t have to wait for your doctor to bring it up. Here’s what you can do:- Bring your full med list to every appointment-even the OTC pills and supplements.
- Ask: “Is this still needed? What’s it doing for me now?”
- Ask: “If I stopped this, what would I watch for?”
- Ask: “What’s the goal of this drug? Is it still relevant?”
- Don’t be afraid to say: “I’d like to try going without this one.”

Elizabeth Grace
I used to be the person who took every pill they handed me until my grandma had a fall and we realized half her meds were from 2012. One day she just stopped the sleep aid and suddenly she was laughing again. No more zombie mode. I wish more doctors asked what we actually want out of life, not just what’s on the checklist.
Steve Enck
The entire premise of deprescribing is predicated upon an ontological fallacy-that pharmaceutical interventions are inherently provisional, when in fact, they are epistemological artifacts of a biomedical paradigm that conflates intervention with care. The statistical reduction in pill count does not equate to improved ontological well-being. Furthermore, the absence of longitudinal mortality data renders these studies statistically inconclusive at best and ideologically motivated at worst.
Jay Everett
Y’ALL. I just read this and I’m crying. Not because it’s sad-because it’s SO OBVIOUS. My dad was on 14 meds. We stopped the statin, the PPI, the muscle relaxant, and the antihistamine he didn’t even know he was taking. He started walking to the mailbox again. He remembered his grandkid’s birthday. This isn’t medicine-it’s liberation. 🙌
Doctors need to stop being scared of saying ‘we don’t need this anymore.’ Patients are begging for it. We just don’t know how to ask.
मनोज कुमार
Polypharmacy is a systemic failure of healthcare economics not clinical practice. Guidelines are irrelevant when reimbursement incentivizes prescribing not de-prescribing. Stop treating symptoms and fix the system
Zed theMartian
Oh wow. So we’re just going to stop giving people medicine because it’s ‘too much’? Next you’ll tell me we should stop giving insulin to diabetics because ‘they’re old now’. This is dangerous nonsense wrapped in feel-good language. You don’t get to cherry-pick which drugs matter based on how ‘awake’ someone feels. Medicine isn’t a buffet.
Ella van Rij
So… we’re now calling it ‘deprescribing’ instead of ‘stopping things that don’t work and might kill you’? Cute. I bet the pharmaceutical reps loved this rebrand. ‘Oh honey, it’s not withdrawal-it’s a *de-prescribing journey*.’ 🙄
Also I misspelled ‘proton’ in my notes once and now I think I’m allergic to PPIs. Just saying.
ATUL BHARDWAJ
In India many elderly take 5-6 medicines without review. Family members forget. Doctors assume they are taken. No one asks. This is global problem not just western
Steve World Shopping
Let’s be real-this isn’t medicine. It’s wellness culture creeping into clinical practice. You think your grandma feels better because you took away her pills? She’s probably just sedated less. That’s not healing. That’s chemical neglect. Real medicine doesn’t fear responsibility. It embraces it-even when it’s hard.
Rebecca M.
I’m just here waiting for the TikTok trend: #DeprescribingDiaries. You know it’s coming. ‘Day 3: I stopped my blood pressure med and now I can see my own face in the mirror again 💆♀️💊 #LifeChanging #MedicationFree’
Meanwhile, my aunt is in the ER because her BP spiked. Guess who didn’t get the memo?
Alicia Marks
This gave me hope. My mom is 80 and I’ve been too scared to ask about her meds. But now I know it’s okay to say: ‘Mom, what if we tried going without this one?’ I’m printing the checklist. Thank you.
Shannara Jenkins
I’m a nurse who’s seen this play out a hundred times. One of my patients stopped his antidepressant after 15 years-thought he’d crash. Instead, he started gardening again. Said he finally felt like himself. Not ‘better.’ Not ‘less drugged.’ Just… himself.
Deprescribing isn’t taking away. It’s giving back. The time, the clarity, the dignity. I wish every doctor had to sit with a patient like this before they write another script.