Understanding Nasal Inflammation and How to Manage It
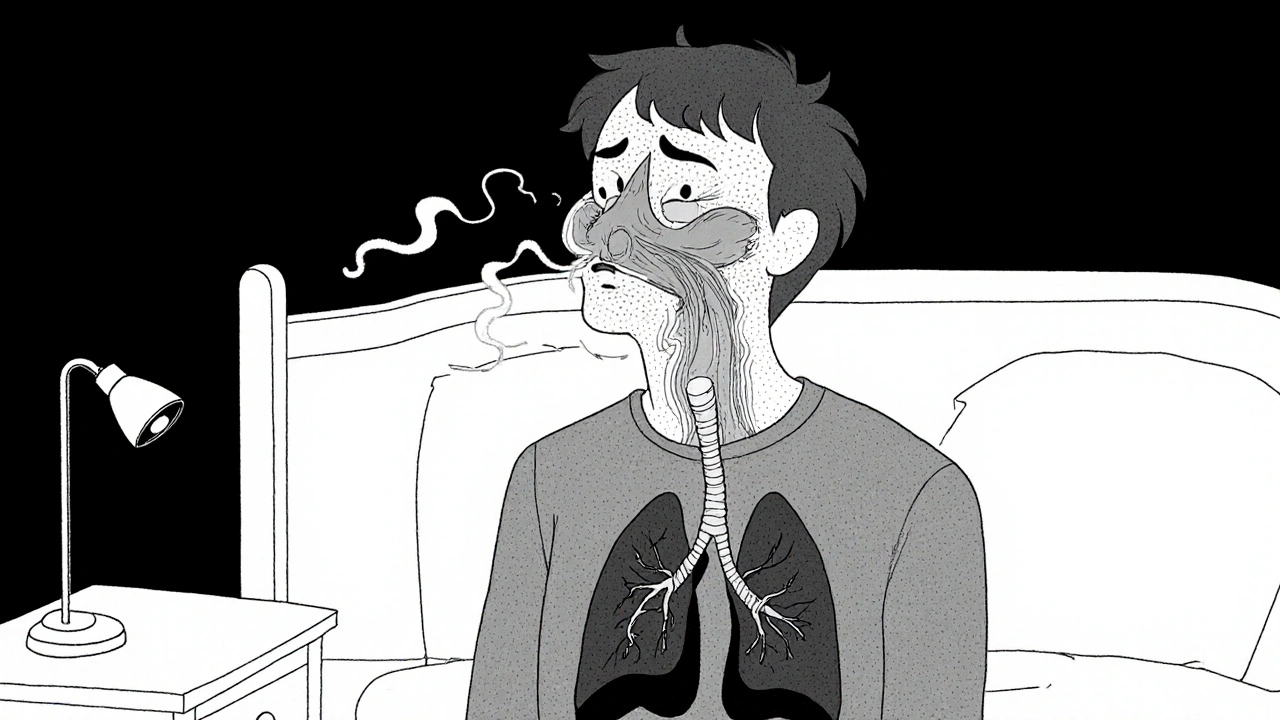
When dealing with Nasal Inflammation, the swelling and irritation of the nasal lining that leads to congestion, runny nose, and facial pressure. Also known as nasal congestion, it often shows up after a cold, during allergy season, or when the air is unusually dry. This condition isn’t just a nuisance; it can affect sleep, concentration, and overall comfort. Below we’ll break down the main players that drive this swelling, why some people get it more often, and what you can do today to feel better.
Key Triggers and Related Conditions
One of the biggest drivers of nasal inflammation is Sinusitis, an infection or persistent inflammation of the sinus cavities that often starts with or worsens nasal swelling. When the sinuses fill with mucus, pressure builds and the nose feels stuffy. Another common companion is Allergic Rhinitis, an immune response to pollen, dust, or pet dander that triggers histamine release and swelling inside the nose. Histamine not only makes you sneeze; it also dilates blood vessels, turning the nasal lining red and puffy. Environmental factors like smoke, strong odors, or sudden temperature changes can aggravate both conditions, turning a mild drip into a full‑blown blockage.
To bring the swelling under control, many turn to medication. Inhaled Corticosteroids, anti‑inflammatory sprays such as budesonide that reduce swelling by calming the immune response in the airway lining are a go‑to for chronic cases. They work slower than a decongestant spray but keep the lining calm over weeks, which is great for people with recurring sinusitis or persistent allergic rhinitis. On the faster side, Antihistamines, drugs that block histamine receptors and stop the itch‑sneeze‑runny‑nose chain like fexofenadine (Allegra) give quick relief during allergy spikes. Combining both approaches—using an antihistamine during peak pollen hours and a low‑dose corticosteroid at night—covers the fast and slow pathways of inflammation.
Beyond pills and sprays, lifestyle tweaks matter. Staying hydrated thins mucus, making it easier to clear. Using a saline rinse or a humidifier adds moisture to the nasal passages, preventing the dry crust that can trigger irritation. If you’re a smoker or live with one, cutting down on smoke exposure can cut the irritant load dramatically. Even simple changes like washing bedding weekly reduces dust mites, a hidden allergen that fuels allergic rhinitis year‑round.
When you notice a sudden shift—like severe facial pain, fever, or thick yellow‑green discharge—it may signal bacterial sinusitis that needs antibiotics. Otherwise, most cases improve with the strategies above. Tracking your symptoms in a quick journal (note the weather, pollen count, and any new products you tried) helps you spot patterns and adjust treatment before the swelling becomes chronic.
In the collection below you’ll find detailed articles that dive deeper into each of these topics: from the science behind edema and alcohol’s effect on swelling to practical tips for using budesonide/formoterol at night, and even guides on buying cheap generic antihistamines safely. Use this roadmap to pick the pieces that match your situation, experiment with the suggested steps, and get your breathing back to normal.
How Sinus Infections Trigger Breathing Disorders - What You Need to Know
Discover how sinus infections can worsen asthma, COPD, and sleep apnea, plus practical steps to treat and prevent both issues for better breathing health.