Drug Interactions: What You Need to Know Before Taking Multiple Medications
When you take more than one medication, your body doesn’t just see them as separate pills—it sees a drug interaction, a change in how one drug affects another when taken together. Also known as medication interactions, these can make drugs stronger, weaker, or even turn them toxic. It’s not just about pills either. Things you eat, drink, or take naturally—like grapefruit juice or St. John’s Wort—can trigger the same dangerous reactions.
Take grapefruit juice, a common breakfast drink that blocks an enzyme critical for breaking down many drugs. Just one glass can spike levels of statins like simvastatin to dangerous levels, raising your risk of muscle damage. Timing doesn’t fix it—whether you drink it hours before or after your pill, the enzyme stays blocked for days. Then there’s St. John’s Wort, an herbal supplement many use for mild depression. It doesn’t just fade away quietly. It can slash the effectiveness of birth control, blood thinners, antidepressants, and even some cancer drugs by forcing your body to flush them out too fast.
And it’s not just herbs or fruit. Even over-the-counter painkillers like NSAIDs can team up with blood pressure meds to wreck your kidneys. Anticoagulants for seniors? They’re lifesaving for stroke prevention—but add an anti-inflammatory or even certain antibiotics, and bleeding risk shoots up. Hydroxyzine, often used for anxiety or itching, can mess with your heart rhythm if mixed with other drugs that affect QT intervals. These aren’t rare edge cases. They show up in real lives, every day.
You don’t need to be a pharmacist to protect yourself. Start by asking: "What else am I taking?" That includes vitamins, supplements, and even occasional pain relievers. Keep a simple list—meds, doses, and why you take them—and bring it to every appointment. Pharmacists aren’t just the ones who hand you the bottle—they’re trained to spot these hidden conflicts before they happen. And if you’re on a long-term drug like prednisone, simvastatin, or an antidepressant, don’t assume it’s safe just because your doctor prescribed it. Conditions change. New meds get added. Your body changes. What was fine last month might be risky now.
The posts below aren’t just lists of warnings—they’re real stories of what happens when interactions go unnoticed, and more importantly, how to stop them before they start. You’ll find clear breakdowns of the most dangerous combos, what to do if you’re already taking risky pairs, and how to talk to your care team without sounding alarmist. Whether you’re managing heart health, mental wellness, or chronic pain, the goal is the same: keep you safe, not just treated.
HIV Medications and Antibiotics: Key Interactions You Must Know
HIV medications and antibiotics can clash in dangerous ways, affecting treatment success and safety. Learn which combinations to avoid, which are safe, and how to check interactions before taking any new drug.
Carbamazepine Generics: Understanding Enzyme Induction and Drug Interactions
Carbamazepine generics can cause dangerous drug interactions and unpredictable blood levels due to enzyme induction. Learn why switching brands can trigger seizures, how to stay safe, and what tests you need.
How to Read Prescription Labels to Avoid Dangerous Drug Interactions
Learn how to read prescription labels to spot dangerous drug interactions. Avoid hospitalizations by understanding warnings, decoding medical jargon, and checking for supplement risks.
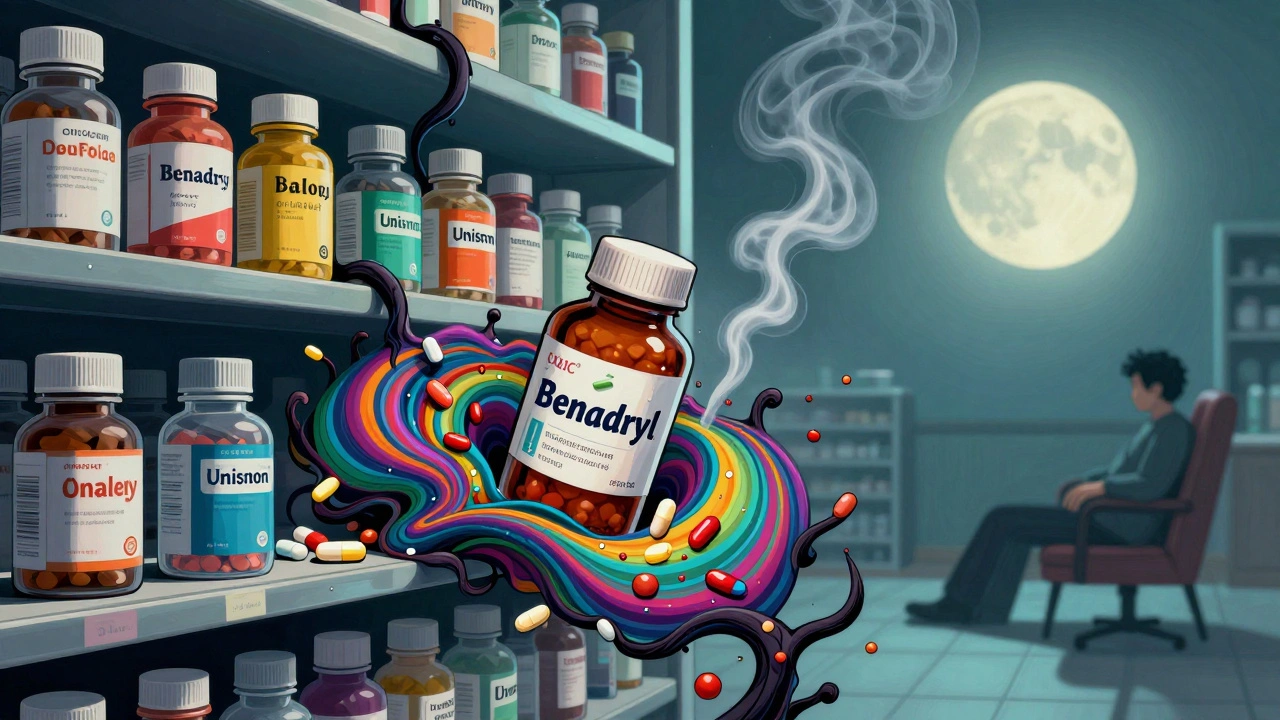
Opioids and Antihistamines: The Hidden Danger of Combined Sedation
Mixing opioids with common antihistamines like Benadryl can cause life-threatening sedation and breathing problems. Learn why this dangerous combo happens, who’s at risk, and how to stay safe.